Plum Health Blog
Coronavirus Update for Detroit Michigan
My name is Dr. Paul Thomas and I'm a Family Medicine Doctor in Detroit, Michigan with Plum Health DPC and this is my update for the Coronavirus as of Saturday April 4th.
Which Counties Nationwide Have been Impacted the Most by Coronavirus?
From the perspective of the number of cases and the number of deaths, the following Counties have been impacted the most by the coronavirus:
New York City (Queens, Bronx, Manhattan, Brooklyn, Staten Island)
Wayne County, Michigan
King County, Washington
Orleans County, Louisiana
Cook County, Illinois
Oakland County, Michigan
Bergen County, New Jersey
This comes from the Johns Hopkins Coronavirus Resource Center and it's notable that Michigan has two neighboring counties in the top 6 hardest hit counties - Wayne County and Oakland County.
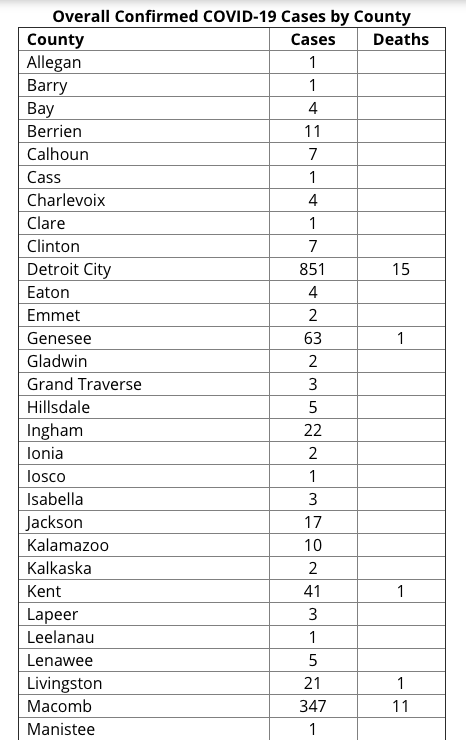
What are the current number of cases and deaths from Coronavirus in Michigan?
Currently, there's 12,744 Coronavirus cases in Michigan and 479 deaths from the Coronavirus in Michigan. What's most troubling about this is the rapid and almost exponential growth of cases here in Michigan. We've seen cases doubling every 2 to 4 days, and that trend does not look like it's slowing down any time soon. That's why it's so crucial that we socially distance our selves to stop the spread of the coronavirus from person to person.
The alarming increase in new cases is also why the CDC now recommends face masks for individuals in the community.
Why Has Michigan and Southeast Michigan Been Hit So Hard by the Coronavirus?
Bridge Magazine wrote an excellent article on this and I agree with their assessment with one addition that we haven't been talking about.
In the article, Bridge Magazine talks about the following factors causing Michigan to be more susceptible to the virus:
Automotive trade with suppliers in Wuhan China
Detroit Metro Airport with Direct Flights to Wuhan, China
Michigan’s March 10th Presidential Primary
Ties between Detroit and Italy via Fiat Chrysler (FCA)
In addition to these factors, I would want to add a few others, including higher rates of overweight and obesity in Detroit and Michigan - rate of overweight is 47.5% in Detroit (34% in NYC) and rate of obesity is 34.6% in Detroit (22% in NYC).
All of these factors have lead to a higher case fatality rate here in Detroit and Michigan than the national case fatality rate:
National Case Fatality rate is 2.47%
Michigan Case Fatality rate is 3.75%
Detroit Case Fatality rate is 3.29%
What are the Comorbid Conditions Increasing the Risk of Mortality in Covid-19 positive patients?
This week, I spoke with a physician colleague at one of the nearby regional hospital systems and we discussed the conditions that lead to a higher mortality rate. These comorbid conditions are as follows:
Cardiovascular disease (High blood pressure)
Diabetes
Pulmonary Disease
Obesity
Cancer
These factors that we discussed were similar to those studied in Wuhan China.
Why are African Americans disproportionately affected by Coronavirus?
African Americans in Detroit and Michigan have been disproportionately affected by the coronavirus. Even though African American people make up only 13.8% of the population in the State of Michigan, 35% of the Coronavirus cases and 40% of the Coronavirus deaths have been experienced in the African American community.
Coronavirus Cases by Race in Michigan. This according to Michigan.gov/Coronavirus. Note the higher rates of infection and mortality in the African American community relative to the population. African Americans make up 13.8% of the population in the State of Michigan.
While it’s still too early to state exactly why this is the case, I have a few theories. First, African American folks have higher rates of diabetes, hypertension, and obesity than their white counterparts here in Detroit and in Michigan. As we stated above, these are risk factors for higher mortality from the Coronavirus. Next, African American people may be more likely to depend on low and minimum wage jobs that put them at a higher risk of contracting the Coronavirus.
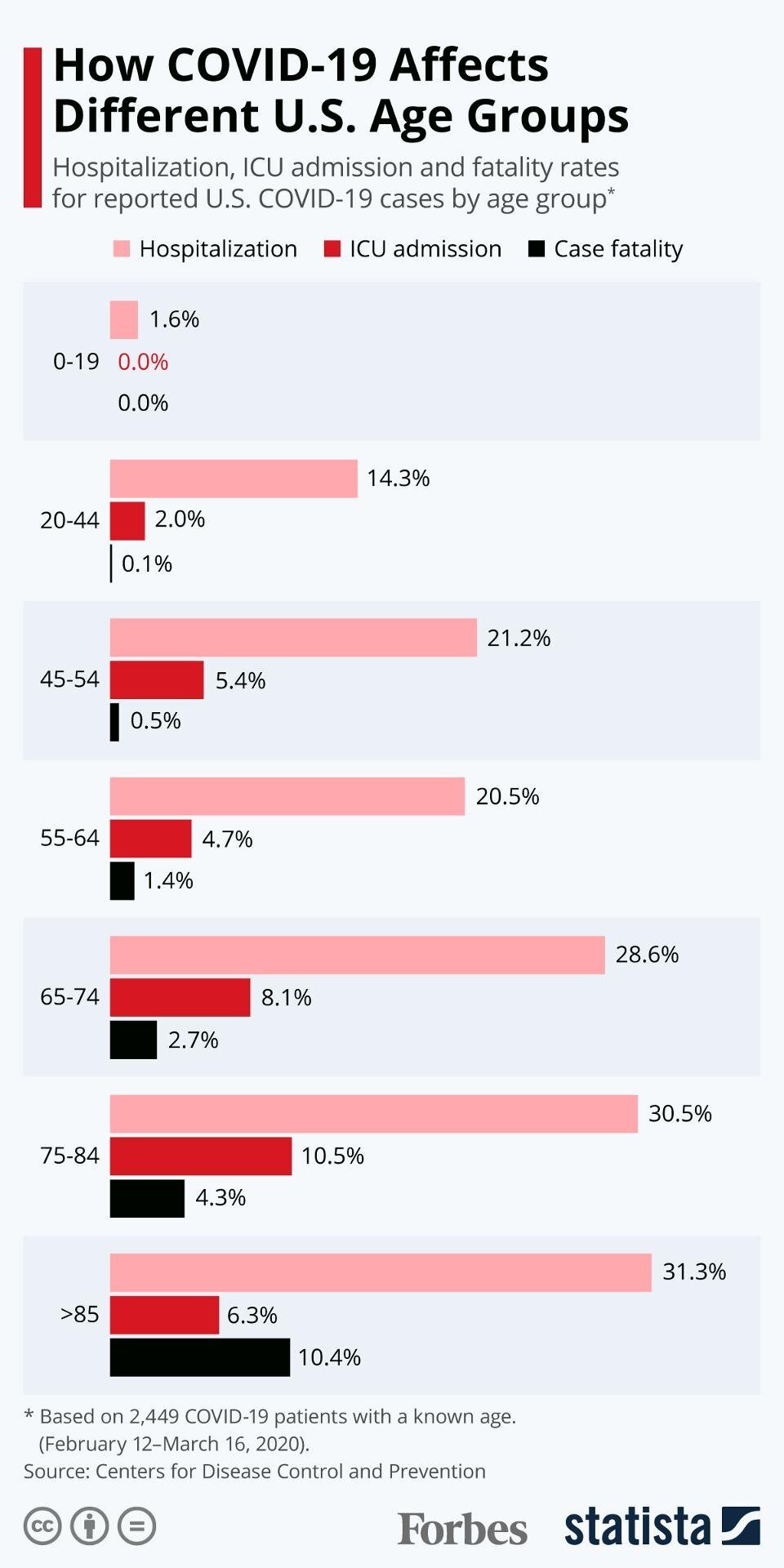
What is the Hospitalization Rate for Covid-19?
Currently, the hospitalization rate for Covid-19 is about 20% or only 1 in 5 people who get the coronavirus will require hospitalization. However, the rates of hospitalization increase with age, meaning that the older the patient, the more likely that they’ll need to be hospitalized for the Coronavirus. That’s why it’s so important to avoid visiting elderly and vulnerable residents in our community.
The older the patient, the more likely it is that they’ll require hospitalization for management of their Coronavirus infections.
Unfortunately, there is a very high mortality rate once a patient needs to be placed on a ventilator. According to studies out of Wuhan, China, the Mortality rate from Coronavirus is 62% among critically ill patients with COVID-19 and the Mortality rate from Coronavirus is 81% among those requiring mechanical ventilation. That means that if you require mechanical ventilation, only 1 in 5 Covid-19 positive patients will come off of the ventilator.
Limited Availability of Ventilators in Michigan Hospitals
The rapid increase in the number of coronavirus patients and the increasing demand for ventilators is putting hospitals, doctors, and nurses in a terrible situation. We’ve now reached the point where doctors are having to decide who lives and who dies from Coronavirus based on ventilator availability. I spoke with a colleague at a large hospital in the Detroit area who relayed that there were only two ventilators for the hospital remaining and that treatment decisions were being made based on comorbidities.
This is a very sad day because we should have never gotten to this point. If we had a functioning Federal Government with a coordinated response and if we had forward-thinking hospitals with greater capacity for disasters like this, we in the medical community wouldn’t have to be making these terrible life and death decisions based on lack of supplies and equipment.
Should I Wear a Mask to Prevent the Spread of the Coronavirus?
Yes, the CDC now recommends that all Americans wear a mask when in a place where they have a higher chance of contracting the Coronavirus, like grocery stores. This can be a cloth or fabric mask. Please wash these each day if you wear them. Please do not horde surgical or N95 masks as these are needed at hospitals at this time.
What can you do to slow down the Coronavirus?
Stay at home
Donate extra supplies to hospitals or your primary care doctor’s office
Unused N95 Masks
Unused Nitrile Gloves
Donate Blood
DO NOT congregate in large groups
DO NOT visit elderly or vulnerable relatives, even if you feel fine
Act as though you have the virus
Thanks for reading and watching, and have a wonderful day,
-Dr. Paul Thomas with Plum Health DPC
Can Vitamin C Treat the Coronavirus?
Can Vitamin C Treat the Coronavirus?
No.
At this time, there is no evidence that Vitamin C can prevent or treat the Coronavirus.
In late March, I began to receive an uptick in questions about vitamin supplementation. There is little to no evidence that high doses of vitamin C will prevent or treat the Coronavirus. But some people have been recommending these supplements as a panacea for all viruses and all seasonal afflictions. There’s also been a few social media posts promoting vitamin supplementation as a cure for Coronavirus. In this blog post, I aim to set the record straight on vitamin C and Coronavirus.
What is Vitamin C?
First of all, Vitamin C (ascorbic acid) is an essential nutrient as it supports normal growth and development and it helps your body absorb iron. Your body doesn’t produce or store vitamin C, so it’s important to get enough vitamin C by eating a healthy diet.
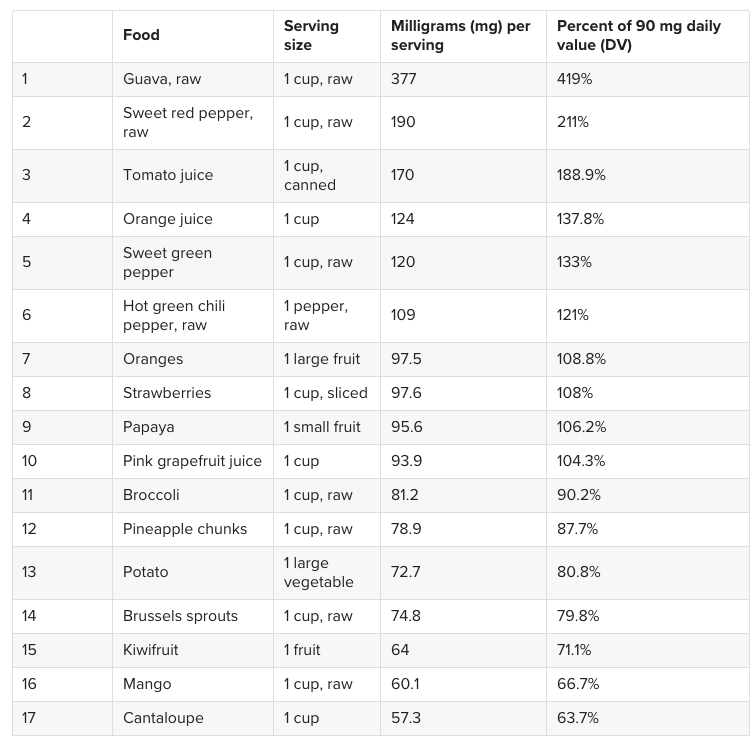
Next, and according to the Mayo Clinic, the average adult needs 65 to 90 mg of vitamin C each day. Again, we can get enough vitamin C by eating a healthy, well-balanced diet. There’s 190 mg of vitamin C in a raw sweet red pepper and there’s 97.5 mg of vitamin C in a large orange. Other foods high in vitamin C include guava, tomato juice, orange juice, strawberries, papayas, and broccoli.
Here’s an awesome chart from Medical News Today that shows which foods are rich in Vitamin C.
The best way to get enough Vitamin C? A healthy diet. The above foods have adequate amounts of Vitamin C.
Where is this Bad Advice on Vitamin C coming from?
Here’s the issue, in late March I was forwarded general advice from a holistic doctor who went so far as to recommend as much vitamin C “as your body can handle” but at least 3,000 to 5,000 mg each day. In their words, this would protect you from the Coronavirus.
Not only is this person misleading their patients and giving potentially dangerous medical advice on a non-individualized basis, but he is also profiteering on their lack of knowledge. The doctor has an online supplement store where patients can purchase his recommended vitamins without a prescription for a hefty sum.
This email was forwarded to me from a holistic doctor who has been prescribing the above supplements as Coronavirus “protection.” As a family medicine doctor who follows evidence-based guidelines, it is very frustrating to see this type of bad information circulating via email and on social media channels.
Can Too Much Vitamin C be Dangerous?
When people think of vitamins, minerals, and supplements, they think of good health. If supplements are good, then more supplements are better, right? But what people don’t know, and what this vitamin-pushing doctor should know, is that mega doses of supplements can have negative consequences.
Most adults only need 65 to 90 mg of vitamin C each day, and adults shouldn’t take more than 2,000 mg each day. Although too much dietary vitamin C is unlikely to be harmful, mega doses of vitamin C supplements might cause diarrhea, nausea, vomiting, heartburn, abdominal cramps, headaches, and insomnia.
Let’s create a hypothetical patient who is a middle-aged adult man who takes Metformin 500 mg twice daily for his long-standing diabetes. The Metformin works well, keeping his blood sugar and hemoglobin a1c levels near normal. It’s important to know that adverse effects of Metformin include diarrhea, GI complaints, nausea, vomiting, and abdominal distention.
If both the Metformin and the high-dose Vitamin C are taken at the same time, the side effects from Vitamin C supplementation may be incorrectly attributed to the Metformin, potentially causing the patient to stop a beneficial medication.
Always Talk to Your Doctor about Your medications and your supplements
It’s entirely possible that in some cases, a patient might be taking mega doses of vitamin C, and not inform their physician of these supplements. Usually a doctor only asks their patients about which medications they’re taking, and not specifically about supplements. If the doctor doesn’t know about these mega doses of vitamins, those adverse effects caused by the vitamin C mega doses may be blamed on or attributed to a life-saving or life-prolonging medications prescribed by your doctor.
And this is just one example - many medications, from blood pressure medications to SSRIs for depression to other medications for diabetes like glipizide can have gastrointestinal side effects. So, please, talk with your family medicine doctor or internal medicine doctor about the medications and supplements that you’re taking.
What Can You do to help improve your immune system?
Here’s my recommendation for a healthy lifestyle during this time:
Exercise: 1 hour daily
Sleep: 7 - 9 hours daily
Eat: a balanced, healthy diet
Meditate: 30 minutes to 1 hour daily
If you choose to supplement with Vitamin C, talk with your doctor.
As a final note, the USA Today wrote a good article about this topic, and Harvard Health has another good article about this topic.
Thanks for reading, - Dr. Paul Thomas with Plum Health DPC
Coronavirus Update March 26th for Detroit Michigan: Can you be Immune to the Coronavirus?
Coronavirus Update March 26th for Detroit Michigan
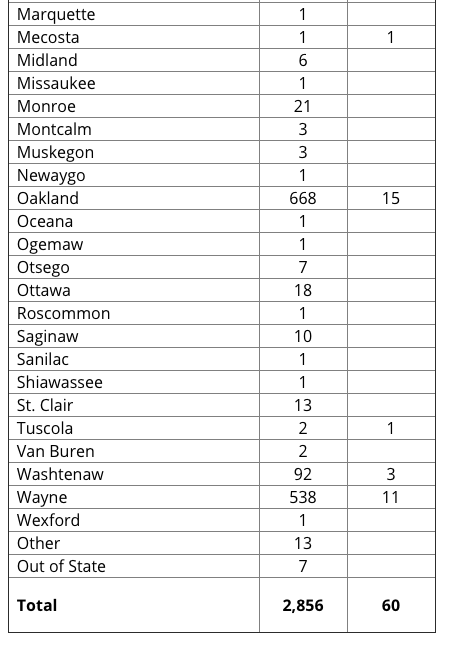
The Coronavirus continues to spread in Michigan. As of today at 2 pm, the Michigan Department of Health and Human Services has reported that there have been 60 deaths and 2,856 cases. That is a mortality rate of 2.1% as of today.
The Coronavirus is concerning for so many reasons, but the two biggest reasons are the rate of transmission and the mortality rate. The Coronavirus spreads, on average, to 2.5 to 2.9 people once an individual is infected. Also, the global mortality rate has been in the 3 to 4% range. Compared to the Flu, these numbers are staggering. The Flu has a rate of transmission of 1.3 and a mortality rate of 0.1%. That makes the Coronavirus 30 to 40 times more deadly than the flu.
Below are the number of cases by Health Department here in Michigan and the number of deaths by Health Department. Detroit is within Wayne County, but it has its own health department, so those numbers are separate from Wayne County Cases.
How Many People Have Tested Positive and How Many People Have Tested Negative?
The State of Michigan today released their data regarding positive tests and negative tests.
30 of 744 outpatient tests have been positive, or a rate of 4.03% at the doctor’s office
1866 of 5261 hospital-based tests have been positive, or a rate of 35.4% at the hospital
557 of 3104 health department cases have been positive, or a rate of 17.9% at the health department
This tells us that if you’re well enough for your doctor to test you at the office and send you home, you are unlikely to have the Coronavirus. It also tells us that if you’re sick enough for your doctor to direct you to the hospital and you meet the testing criteria at the hospital (fever, cough, potential exposure), then you have a good chance of testing positive at 35.4%. This information can be found on the MDHHS Website.
Data from the Michigan Department of Health and Human Services showing the number of positive and negative tests in the State of Michigan as of 03/25/2020.
Hospital Beds are Filling up in Detroit
According to this article in the Detroit Free Press, the Beaumont Hospitals in Detroit and West Bloomfield are filling up with patients.
The health system is "facing limitations and nearing capacity with our testing, personal protective equipment and mechanical ventilators," said Beaumont Health Chief Operating Officer Carolyn Wilson. “We are taking steps to increase our capacity, such as converting some of our operating rooms into intensive care units.
“We have been actively transferring COVID-19 patients within our system to other Beaumont hospitals, as appropriate, if one hospital has more capacity than another."
According to this article in the Detroit News, Henry Ford Health System is facing the same challenges.
"Today our capacity is quite full at those two hospitals — West Bloomfield and Henry Ford Hospital in Detroit," said Dr. Betty Chu, associate chief clinical officer and chief quality officer. Chu is leading the health system's coronavirus response.
"We fortunately have the luxury right now of having additional capacity at some of our other campuses."
This is concerning because there are a limited number of staff, beds, and equipment to adequately are for Coronavirus patients here in the Detroit and Metro Detroit area.
As beds fill up and as our hospital personnel are stretched thin, we may be in a situation where doctors have to pick who lives and who dies simply based on issues of capacity. This is truly a terrible situation and one that we want to completely avoid.
That is why it’s so important to stay at home and avoid any unnecessary contact with people, by which you may become infected.
City of Detroit Will Begin Offering Free Coronavirus Testing Tomorrow
Unfortunately, the City of Detroit has been hit hard by the Coronavirus. But, Mayor Mike Duggan and the City of Detroit will begin testing people at the State Fairgrounds at 8 mile and Woodward to hopefully stem the tide. The aim is to test 50 people every hour and 400 people every day with this drive-through testing.
Testing is important because it can help us track the spread of infection and it can help people prevent the spread by self-quarantine if they find out that they are infected. You can learn more about this testing via the City of Detroit, here.
How Can I Become Immune to the Coronavirus?
Yes, you can become immune to the Coronavirus. When you get infected with the Coronavirus, your body will produce antibodies or immunoglobulins to the Coronavirus. First you’ll make IgM, and then IgG. This will confer long-term immunity to you.
Scientists estimate that you’ll be immune for 1 to 3 years based on previous infection and immunity rates from other Coronaviruses. This is why you can’t get re-infected by COVID-19. Once you have the virus, you’ll be immune to future infection.
This is important for several reasons. Over the next few weeks to the next few months, there will be a test of immunity. It will likely be a finger-stick blood test, using a drop of blood to measure the immunoglobulins like IgM or IgG to make sure folks are immune.
This will be especially important for doctors, nurses, hospital workers, and other critical staff. If we know that these folks are immune to Coronavirus, they can go back to treating patients with minimal risk of infection going forward. This test is pending as of now.
HOw will the Coronavirus Pandemic End?
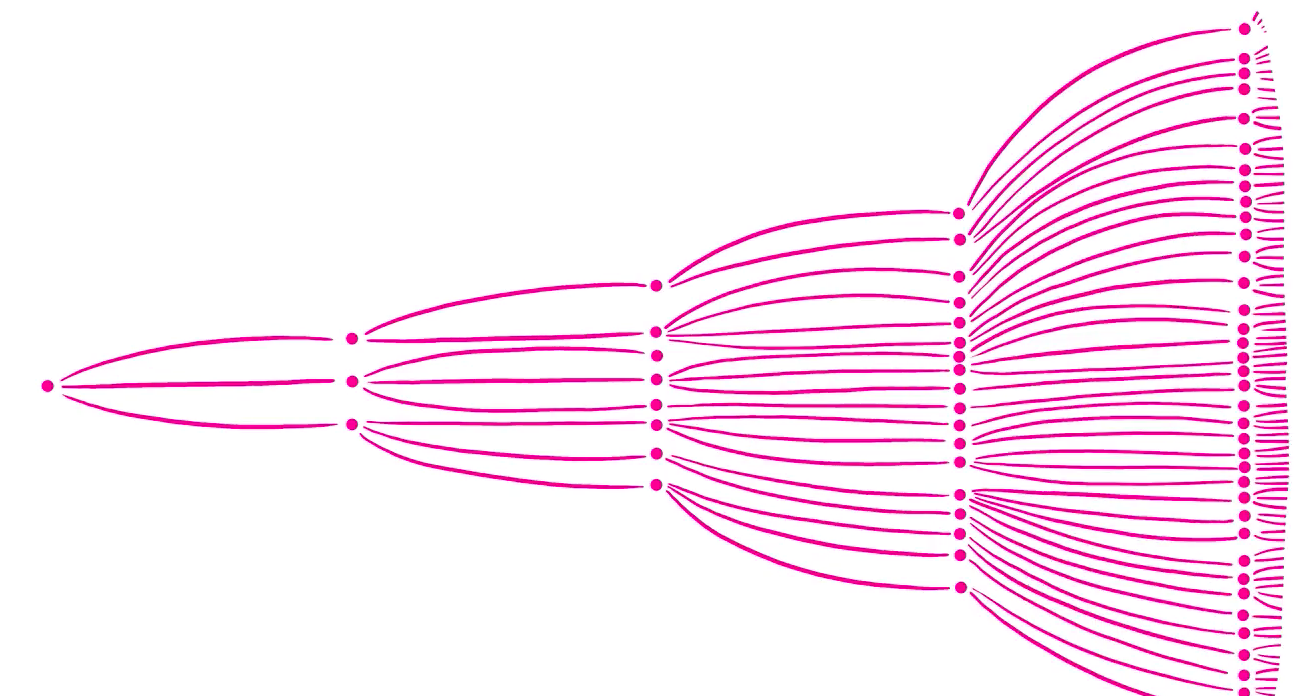
The Coronavirus pandemic will end when we reach a Herd Immunity. Herd Immunity means that enough people in the population are immune to the Coronavirus, which will greatly limit its spread.
This Herd Immunity can be achieved in a few different ways. First, once a number of Americans get the Coronavirus, they will fight off the infection and become immune, limiting the spread of the virus once they recover. Second, once a vaccine is developed, many more people will become immune through vaccination.
Just like being vaccinated for the influenza virus or for Measles, Mumps, and Rubella, once you’re vaccinated for these viruses, your body creates immunoglobulins or antibodies to help protect you from infection from these viruses.
Unfortunately, the Coronavirus or COVID-19 vaccine will take 18 months to 2 years to develop, so this option will take a long time to achieve.
This image demonstrates Herd Immunity. The left hand panel shows what we’re dealing with right now with the Novel Coronavirus or COVID-19. No one is immune to this COVID-19 yet. The right hand panel shows Herd Immunity. The yellow figures are immune to the virus, so the spread of the virus will be limited. Herd Immunity defined: the resistance to the spread of a contagious disease within a population that results if a sufficiently high proportion of individuals are immune to the disease, especially through vaccination.
Thanks for reading and watching. Please stay safe and healthy in this time,
-Dr. Paul Thomas with Plum Health DPC
Single Largest Jump in Coronavirus Cases in a 24 Hour Period
Coronavirus Update: United States sees the single biggest increase in cases in a 24 hour period
Unfortunately, the United States has just witnessed the single largest increase in Coronavirus cases of any country in a 24 hour period. Over the last 24 hours, there have been 14,550 new cases reported in the United States according to this website.
Why is the Coronavirus Spreading so quickly in the United States?
It comes down to the concept of R⌀.
R⌀ is the average number of people that an infected person transmits the virus to.
If R⌀ is <1, the epidemic will burn out.
If R⌀ = 1, then epidemic will continue at a steady pace.
If R⌀ >1, the epidemic will increase exponentially.
Current estimates put R⌀ at about 2.5 to 2.9 (Peng PWH et al, 2/28). In plain English, this means that the average person with the Coronavirus will give the virus to 2.5 to 2.9 other people. This transmission rate is a bit higher than seasonal influenza. R⌀ is a reflection of both the virus and also human behavior. Interventions such as social distancing and improved hygiene will decrease R⌀.
Control of spread of COVID-19 in China proves that R⌀ is a modifiable number that can be reduced by effective public health interventions. The R⌀ on board the Diamond Princess cruise ship was 15 – illustrating that cramped quarters with inadequate hygiene will increase R⌀ (Rocklov 2/28).
The Coronavirus started with a single infected person, and it spread to roughly 2.5 to 2.9 other people. Once infected, those people passed the Coronavirus to another 2.5 to 2.9 people each. This is how a virus can exponentially spread. The Coronavirus spread has been hard to diminish because people have a relatively long incubation period or they have the virus and they don’t show symptoms of having the virus for a relatively long period of time, like 5 days to 10 days.
What should I be doing during the Coronavirus pandemic?
Definitely stay at home as much as possible. If you must go outside your home, practice social distancing and act as though you have the virus. Essential tasks done outside the home include buying groceries, making visits to the doctor, and picking up medications from the pharmacy.
How do I protect myself when I go outside?
First, avoid going outside unless you’re going for a walk or otherwise exercising in your neighborhood. If you must go outside, wear disposable latex gloves when you touch high-risk surfaces. For example, when you pump gas at the gas station, put on a pair of latex gloves during the credit card use, key pad entry, and handling the gas pump. Then, dispose of the gloves responsibly in a nearby trash can. Use hand sanitizer once you’re back in your car. Don’t touch your eyes, nose, or mouth after touching potentially contaminated surfaces. You can also use this routine of wearing latex gloves when grocery shopping or when handling a grocery cart.
Is it safe to get food delivered?
Yes, it’s safe to have food delivered and it’s safe to get take-out food. The best practice is to wash your hands after touching any packaging and to wash your hands again before eating. For instance, if you get your food in a brown paper bag, take your food out of the brown paper bag, recycle or discard the brown paper bag, and wash your hands before touching the food or individually wrapped food. Then, transfer the food to a plate or glass bowl and microwave the food for 30 seconds. This will kill any germs or bacteria in or on the food. Wash your hands again prior to eating.
What can you do to boost your immune system?
Many people want to know what they can do to boost their immune system to protect themselves from the Coronavirus. You can do the following to boost your immune system:
Sleep 7 to 9 hours each nigh
Eat nutritious and healthy foods
Drink plenty of fluids, mostly water
Exercise for 1 hour each day
Meditate to keep your stress levels low
When we’re stressed out, we tend to produce more cortisol, a steroid hormone that can weaken our immune system. That’s why it’s important to meditate, sleep well, and exercise.
What are good exercises during the Coronavirus quarantine?
You definitely want to exercise every day during the Coronavirus quarantine. Exercise will be good for your physical health, immune system, and emotional wellbeing. The best exercises will be to go outside of your house for a walk, jog, run, or bike ride. This is one of the few exceptions to the “stay at home” rule above. When you exercise, make sure that you’re keeping your distance from other people by at least 6 feet. You can exercise in your neighborhood or a nearby park. Avoid mall walking or any exercise where you’ll have to open a door/use a door handle for entry. That’s why we recommend folks avoid gyms and pools because there are just too many surfaces that could harbor the Coronavirus and potentially spread the infection. Therefore, exercise at home: lift weights, do floor exercises, do yoga or pilates. Fortunately, several health and fitness companies are giving free 30 day trials of home exercises - take advantage of these programs.
What can you do to slow down the Spread of Coronavirus?
Stay at home.
Act as though you have the virus and any interaction is a potential to spread the virus to a vulnerable person. People who are the most vulnerable are older adults or those with pre-existing medical conditions like lung diseases or cardiovascular diseases.
Do not visit nursing homes or elderly relatives, even if you feel well. You could be an asymptomatic carrier of the coronavirus and you could potentially endanger or kill the older adults that you visit.
Should you be sitting on a stockpile of extra medical supplies and equipment, please donate it to your nearest hospital or primary care physician office. If you have new and unused N95 masks or gloves, please donate them to these healthcare facilities.
Thanks for reading and watching, and have a wonderful day.
-Dr. Paul Thomas with Plum Health DPC
Detroit Doctor on AskASwimPro Show with Fares Ksebati
This week, I was invited on the AskASwimPro Show with Fares Ksebati. Fares is the CEO of MySwimPro, an App that helps swimmers improve their stroke, among other things. From their website:
MySwimPro is using technology to advance the sport of swimming and help swimmers all over the world achieve their goals in new and exciting ways. The platform is more than just an app, it's a community that keeps you accountable and pushes you to do your best.
In general, we had an informative discussion about the Coronavirus and its impact on our communities, specifically swimmers. Here’s what the MySwimPro team wrote about on their blog, found here:
In this episode of the #AskASwimPro Show, we interviewed Dr. Paul Thomas of Plum Health about the novel coronavirus, how to practice social distancing, the importance of “flattening the curve” and how swimmers can stay safe.
Dr. Thomas explained that many of us have had a coronavirus before, but that COVID-19 is more contagious. COVID-19 has a mortality rate of 3.5%, compared to the seasonal flu’s mortality rate of 0.1%, he says.
The virus spreads through coughing and inhaling someone else’s respiratory droplets. Due to this, Dr. Thomas explained that it isn’t wise to fly right now, since airplanes place you in close proximity to others.
He also noted that COVID-19 can live on surfaces for up to 3 days:
Stainless steel and plastic: 3 days
Cardboard and paper products: 24 hours
Copper: 4 hours
We go on to discuss social distancing:
Social distancing involves staying 6 feet away from others when you are outside, and avoiding contact with others while at home. You risk transmission any time you talk, shake hands or spend time around others. Dr. Thomas recommends that people avoid gathering with others and stay home in “self-quarantine,” noting that in cultures where it is common to kiss each other on the cheek or shake hands, COVID-19 can spread very quickly.
If you get COVID-19, you will be quarantined for at least 14 days, Dr. Thomas said. However, researchers have mentioned that you may be able to infect others for up to 20 days after showing symptoms.
We then discuss Flattening the Curve:
The healthcare system in the United States can only manage so many patients at one time, Dr. Thomas said. By practicing social distancing, we can “flatten the curve,” reducing the number of COVID-19 cases at a given time and keeping healthcare providers within their capacity. If we don’t do this, Dr. Thomas noted that the U.S. healthcare system will be unable to effectively care for patients.
We then talked about how you can stay safe during this Coronavirus Pandemic:
Dr. Thomas shared tips to stay safe and healthy:
Wash your hands: Before you prepare food, after going to the bathroom and before touching your face.
If you have a cough or a low grade fever (99 or 100 degrees Fahrenheit): Stay home, drink lots of fluids, take Tylenol and get some rest. You likely are not sick enough to benefit from a doctor’s treatment. Save the hospital beds — and the healthcare providers’ time — for those who are sickest!
If you have severe symptoms, such as a high fever and trouble breathing: Go to the hospital.
Thanks for reading and watching,
-Dr. Paul Thomas with Plum Health DPC
Detroit Doctor Answers Questions about Coronavirus on WDET's Detroit Today
Dr. Paul Thomas, MD, a family medicine doctor in Detroit answers many questions that Detroiters have about the Coronavirus and its impact on our community.
From WDET:
Dr. Paul Thomas is a primary care physician at Plum Health direct primary care in Corktown, an office that utilizes a monthly membership to treat patients rather than through insurance. He says that with job security threatened and instability on the horizon it is important to have comprehensive health care not tied to employer-based insurance.
His tips:
Keep a pair of gloves in the car to use at the gas station or grocery store to prevent touching contaminated surfaces when running essential errands.
The virus can live on cardboard for up to 24 hours. For this reason, leave mail out for roughly two days before picking it up.
Swap Tylenol for ibuprofen (based on an evolving scientific study).
To boost your immune system get eight hours of sleep, get some vitamin D when the sun is out and take a long (isolated) walk once a day.
If you are experiencing fever or shortness of breath seek medical treatment at the hospital.
Listen to the full episode, here.
Thanks for reading and listening!
-Dr. Paul Thomas with Plum Health DPC in Detroit Michigan
Flattening the Curve for Coronavirus in Detroit Michigan
Coronavirus is here in Michigan. As of now, there are 53 cases in the State of Michigan. So what can we do to prevent the spread of the virus? What does it mean to practice social distancing? What does it mean to flatten the curve?
What’s the best thing you can do to prevent the spread of the Coronavirus?
The best thing to do to prevent the spread of the virus is to act as if you already have the virus and do everything that you can to prevent transmitting it to your loved ones and vulnerable people in the community.
What is social distancing?
Social Distancing is a term applied to certain actions that are taken by Public Health officials and all of us to stop or slow down the spread of a highly contagious disease. Cancelling events that are likely to draw crowds is an example of social distancing enacted by Public Health officials. Social distancing enacted by us as individuals means deliberately increasing the physical space between yourself and the people in the community. This may look like staying at home away from other people or it may mean keeping a 6 foot space between yourself and other people in the community.
What does it mean to flatten the curve?
To flatten the curve is to decrease the rapid transmission of the Coronavirus and therefore decrease the peak number of actively infected individuals at any one time. This is important because if there are too many infected individuals, we will exceed our hospital bed and ventilator capacity. If we don't flatten the curve, there will be unnecessary deaths due to the spread of the Coronavirus.
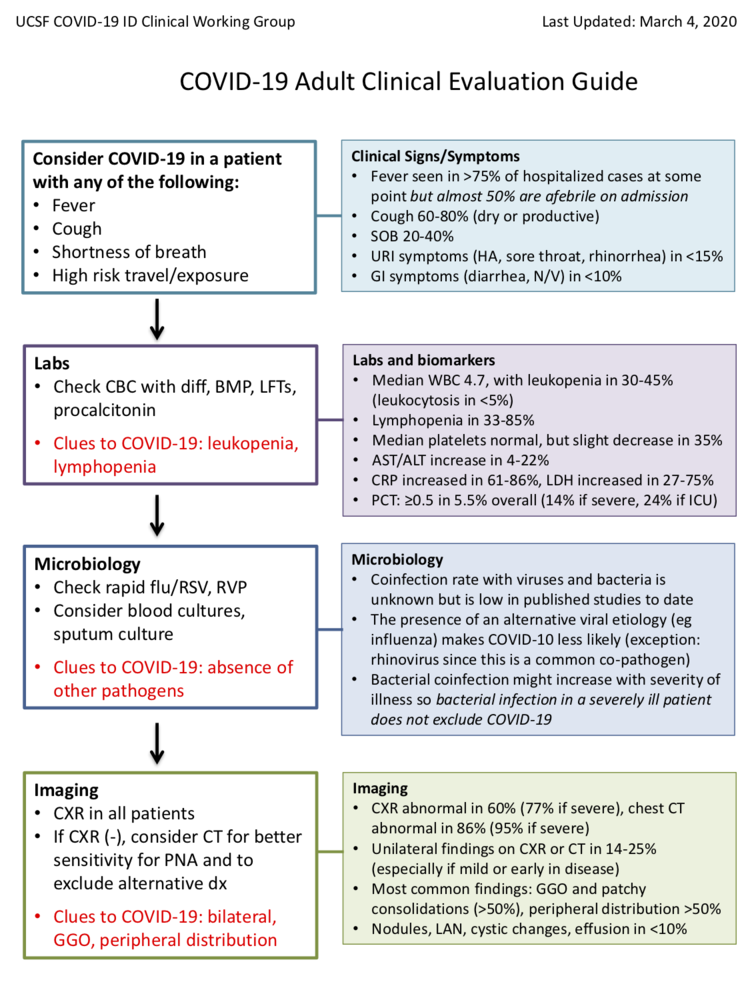
What is the most common presentation for the Coronavirus?
A: The most common presentation for the Coronavirus is a one-week prodrome of myalgia or muscle aches, malaise or generally not feeling well, cough, and low-grade fevers. This gradually leads to more severe trouble breathing in the second week of illness. There is an average of eight days to the development of dyspnea and an average nine days to onset of pneumonia or pneumonitis.
How is the presentation of Coronavirus different from the presentation of Influenza?
A: Coronavirus tends to have a gradual onset. Influenza tends to have a sudden onset. Coronavirus tends to have a cough and fever. Influenza tends to have fever, chills, muscle aches, nausea, vomiting, and diarrhea.
What are the lab findings like for the Coronavirus?
A: The most consistently present lab finding was lymphocytopenia (with either leukocytosis or leukocytopenia). Lymphocytopenia is the condition of having an abnormally low level of lymphocytes in the blood. Lymphocytes are a white blood cell with important functions in the immune system. It is also called lymphopenia. The opposite is lymphocytosis, which refers to an excessive level of lymphocytes. During other infections, we typically see lymphocytosis or an increase in white blood cells to fight off the infection. Aside from the depressed white blood cell count, other markers like C-reactive protein or pro-calcitonin were not as consistent.
What are the most common radiographic findings for Coronavirus?
A: The most consistent radiographic finding, discovered on chest x-ray, is bilateral interstitial infiltrates also known as ground glass infiltrates or ground glass opacities. A radiograph is an image produced on a sensitive plate or film by X-rays, gamma rays, or similar radiation, and typically used in medical examination.
Can you get a co-infection with another virus or bacterial infection when you get the Coronavirus?
A: Co-infection rate with other respiratory viruses like Influenza or respiratory syncytial virus (RSV) is less than two percent. Basically, if you have a positive test for another respiratory virus, then you do not test for COVID-19. This information is based on a large dataset from China.
When people get the Influenza virus, they don’t often die from the Influenza virus, but from a subsequent and opportunistic bacterial infection like a bacterial pneumonia. Is this the case for Coronavirus?
So far, there have been very few concurrent or subsequent bacterial infections, unlike Influenza where secondary bacterial infections are common and a large source of additional morbidity and mortality.
How much does it cost to get the Coronavirus test?
A: It depends on the lab, the health system, and the insurance company. LabCorp is offering a test for roughly $50, Quest Diagnostics is offering a test for roughly $250, and the test may be free for those who have insurance, depending on your symptoms.
What can we do to treat the Coronavirus?
A: To date, patients with severe disease are mostly getting Remdesivir from Gilead through compassionate use. However, the expectation is that avenue for getting the drug will likely close shortly. It will be expected that patients would have to enroll in either Gilead’s randomly controlledtrial or the National Institute of Health’s “Adaptive” randomly controlled trial (Remdesivir vs. Placebo). Others have tried Kaletra, but that medication was not beneficial.
How long are patients contagious after they contract the Coronavirus?
A: The short answer is that patients are likely contagious for 20 days after contracting the Coronavirus. The more complicated answer is that patients can shed RNA from one to four weeks after symptom resolution, but it is unknown if the presence of RNA equals presence of infectious virus. For now, COVID-19 patients are cleared of isolation once they have two consecutive negative RNA tests collected more than 24 hours apart.
Thanks for reading and stay safe out there.
-Dr. Paul Thomas, MD with Plum Health DPC
Coronavirus Update for Detroit Michigan March 2020
Coronavirus Update for Detroit, Michigan for March 2020
I’m a Family Doctor in Detroit, and today I’ve gotten a ton of questions about the Coronavirus - ask me anything!
For starters, here’s what I sent out to all of my Plum Health DPC (https://www.plumhealthdpc.com/) patients earlier today and I thought everyone should know these things as well. Beyond what’s written below, ask me anything:
Plum Pack!
The Coronavirus is causing concern at this time - the President spoke last night about closing access to the USA from Europe, the NBA, NHL, and NCAA have cancelled/postponed all of their games, and other major events have been cancelled - but do not panic.
People Will Become Sick This Spring
Many people will get sick and have upper respiratory symptoms over the next few days and weeks. Most of these will be from the common cold, many of these symptoms will be from seasonal allergies, some will be the flu, and some may be due to the Coronavirus.
What I can do for you is to help you triage - I can help you determine if you're sick with the flu, a cold, or having an allergy flare up. I can help you determine if you have symptoms that are concerning for the Coronavirus.
If you contact me and I'm concerned, I may send you to the emergency department for further testing. As of now, Coronavirus testing is not available at our clinic.
Here are some algorithms about how I approach caring for our patients, caring for all of you.
Additionally, heres information from the State of Michigan regarding Coronavirus, released earlier today:
Finally, below is what we know and what you can do to protect yourself:
What You Can Do to Prepare for the Coronavirus
You can prepare for the Coronavirus by taking several actions and non-actions:
wash your hands thoroughly before eating
wash your hands thoroughly after using the bathroom
wash your hands thoroughly before touching your T-zone (eyes, nose, or mouth)
Cough or Sneeze into the crook of your arm/the bend in your elbow; again, wash your hands after coughing or sneezing
purchase food and supplies in case you need to be self-quarantined
if you become sick with a respiratory infection, but you’re not sick enough to require hospitalization, you may need to self-quarantine or stay at home to avoid infecting your neighbors and co-workers
if you become ill, call your doctor and discuss your symptoms. It may be better to call or text your physician, as going to the doctor’s office may
cancel any non-essential travel to areas where the virus is spreading like China, Iran, South Korea, and Italy
avoid large gatherings - parades, sporting events, campaign rallies - to avoid catching the virus or spreading the virus
What We Know About the Coronavirus or Covid-19
Here’s what we know thus far:
Every single one of us has had a coronavirus infection in the past — it’s one of the viruses (along with rhinovirus, adenovirus, etc.) that causes the common cold. This novel Coronavirus (COVID-19) is just a variation (or mutation).
This new coronavirus can cause anything from nothing to a mild cold to a potentially lethal viral pneumonia.
Those who seem to be most affected by COVID-19 thus far are those who are more at risk to begin with: those who are older, those with multiple chronic health conditions, etc.
The evidence out of the initial outbreak in Wuhan, China revealed:
Median age = 59 years of age
Estimated basic reproduction number (the number of people an infected person infects) is approximately 2.2
The average length of time from the onset of symptoms to hospitalization was 9.5 to 12.1 days
There have been new coronaviruses in the past — most notably the SARS (2002, 2003) and MERS (2012 – Present) epidemics; however, the mortality rate of COVID-19 (2.0% to 4.0% or below) is notably lower than SARS (9-10%) and MERS (36%).
From the WHO, they estimate that the mortality rate is somewhere around 3 - 4%. We are more concerned about this Coronavirus than the typical flu virus because of this higher mortality rate. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200306-sitrep-46-covid-19.pdf?sfvrsn=96b04adf_2
This virus spreads from person to person, though we aren’t exactly sure how. Our best hypothesis is that it is spread via bodily fluids and droplets from speaking, breathing, coughing, sneezing, etc (and potentially through the GI tract).
Children absolutely can get the Coronavirus that causes COVID-19. Two interesting points about pediatric patients: 1) there is early evidence that they carry a high “viral load” and — combined with the fact that they aren’t great at washing hands, not touching their face, etc. — because of this may be more likely to spread the illness and 2) children who do get COVID-19 seem to have a lower mortality rate than those who are older who contract the disease.
Here’s what we don’t know:
We don’t know if this virus will peter out as the warmer months kick in; we also don’t know if this is a one-season thing or if it will come back strong again next cold & flu season.
We don’t know when or if we’ll have a successful vaccine to prevent against this new virus. In a late February 2020 press conference, Dr. Anthony Fauci did a great job describing how a vaccine is created (starts at about 11:00 into the clip) and how far we are away from a successful vaccine.
How to Protect Yourself and Others from the Coronavirus
How to protect yourself & others:
Just like any other respiratory virus: stay home if you’re sick!
Just like preventing any other respiratory virus: take good care of yourself! Exercise regularly, eat nutritious, balanced meals, practice stress mitigation techniques, and get a solid 7-9 hours of sleep a night, etc.
Just like preventing any other respiratory virus: wash your hands! A lot!
Just like preventing any other respiratory virus: don’t touch your eyes, mouth, nose, etc., and get into the habit of washing your hands before eating.
If you can, avoid contact with those who are sick or are caring for the sick.
If you are not actively sick (or caring for someone who is), ear-loop/surgical masks are not likely helpful. Healthcare workers will wear masks (and often higher-rated ones than the ear-loop masks), as they have a much higher likelihood of caring for someone with the disease and are prioritizing mitigating the spread to others.
Those who are exposed to someone with COVID-19 or those who are being tested for COVID-19 will likely be asked to self-quarantine (currently not mandatory). If your job permits, start asking your employer about work-from-home opportunities; if your job doesn’t permit work-from-home, ask your employer what their plan is to keep you safe!
Because of the real possibility of a quarantine, stock a couple week’s worth of non-perishable foods items in a pantry. Also make sure you have the basics — like medications, OTCs like ibuprofen, acetaminophen, diphenhydramine, and pseudoephedrine, and (a rational amount of) toilet paper, facial tissues, etc.
Dr. Raquel Orlich Reaches A Major Milestone
This week, Dr. Raquel Orlich reached a major milestone - she now has 200 patients in her practice panel. Here’s what we said on Facebook:
A huge congratulations 🎈 to Dr. Raquel Orlich. She joined our Plum Health direct primary care practice on July 1st 2019 and she’s already reached 200 patients in her panel!
Dr. Raquel 👩🏻⚕️ is intelligent, compassionate, and a relentless advocate for the health and wellbeing of her patients. She focuses on chronic musculoskeletal issues, women's health, and preventive medicine.
We’re lucky to work with you, and our patients are fortunate to have such a kind and caring doctor looking out for their best interests. 💯
Of note, Dr. Raquel has room for about 500 patients in her practice panel, so if you’d like to sign up to be one of her patients, head over to our Schedule Now page to get started!
-Drs. Paul Thomas and Raquel Orlich with Plum Health DPC
Do I have the Cold? Flu? or Strep Throat? Answers for People in Detroit Michigan
Do I Have the Cold, the Flu, or Strep Throat?
Dr. Paul Thomas and Dr. Raquel Orlich are family medicine physicians in Detroit Michigan. Their office is called Plum Health DPC and it’s located on Michigan Avenue in the beautiful Corktown Neighborhood of Detroit, MI.
Many people want to know if their sore throat, body aches, chills, fever, stuffiness, runny nose, or other symptoms are related to the cold, the flu, or strep throat. So, in this blog post and associated YouTube video, we’ll explore the differences between these clinical entities.
How Do I Know if I Have The Common Cold?
People with the common cold have a runny nose, a stuffy nose, congestion, sneezing, and a sore throat. Common cold viruses prefer to affect the back of the throat - these viruses have a predilection for the posterior pharyngeal tissues. This causes your mucus membranes to swell up, which causes fluid to leak out or what you experience as a runny nose or congestion, post-nasal drainage, etc… These symptoms tend to come on gradually.
For this viral pharyngitis or viral upper respiratory system or common cold, antibiotics are not indicated. Antibiotics do not work for the common cold, because the common cold is caused by a virus that mutates rapidly and is difficult to treat. Antibiotics are indicated for bacterial infections, like strep throat and pneumonia.
How Do I Know if I Have Influenza?
Influenza usually presents with extreme fatigue, muscle aches, and a fever. Sometimes we say that there’s an associated “pajama sign” - sometimes people are so weak and so tired that they can’t even change their clothes before coming to the doctor’s office, thus they come to the office in their pajamas. There can also be chest discomfort, chills, and a headache. There is often an abrupt onset to these symptoms. The symptoms of the flu are often more severe, and sometimes fatal unfortunately. This is why we worry more about the flu and why we recommend that everyone gets the flu shot.
If you are positive for an influenza infection, treatment with oseltamivir (Tamiflu) should be started within 24 to 48 hours of your symptoms. It must be started within this timeframe to be effective in shortening the duration of flu symptoms and decreasing the severity of the flu virus.
It’s the Middle of February - Will the Flu Shot Still be Effective?
Yes. We’re still in the influenza season, and the flu shot has been shown to be 40 to 50% effective in preventing the influenza virus from taking hold. So, we strongly recommend getting the flu shot if you haven’t done so already. The flu shot costs $20 at our office and about that price at most pharmacies ($15 - $30). And it’s very important to get the flu shot, not only to protect yourself, but also to protect your loved ones. If you get the flu shot, you’ll be less likely to transmit the flu to a more vulnerable person in your life, like a newborn in your family or circle of friends, or an elderly relative or elderly neighbor. Getting the flu shot helps to protect these more vulnerable people with less strong immune systems from getting the flu.
How Do I Know if I Have Strep Throat?
When people come to our office concerned about a sore throat, it’s hard to tell if it’s a viral pharyngitis or if it’s strep throat (a type of throat infection caused by a bacteria). Strep throat is an infection of the tonsils in the back of the throat by a bacteria, Group A Streptococcus. The “strep” in strep throat comes from a shortening of the bacteria name, Streptococcus. The strep bacteria infects the tonsils and causes localized pain and swelling as well as purulent discharge, ie a discharge of pus from the tonsils.
There’s also a diagnostic criteria for Strep Throat called the Centor Criteria. You get a point for having each of the following symptoms:
fever
tonsillar exudate (pus coming from the tonsils)
absence of a cough (no cough)
anterior cervical lymphadenopathy (swollen and often tender lymph nodes in the front part of the neck)
age younger than 14 years
Kids with a sore throat are more likely to have Strep Throat because they have larger tonsillar tissue when they’re younger. As people age, the lymphatic tissue, like tonsils, shrink in size. This makes it less likely for adults to get strep throat. Of note, the tonsils are like a sponge and they take up large amounts of bacteria and viruses and show it to the rest of our body to make sure that our immune system can respond appropriately to these foreign invaders.
Because Strep Throat is caused by a bacteria, it is appropriate to use antibiotics for this condition. We often use Amoxicillin 500 mg for adults and Amoxicillin with weight-based dosing for children. Fortunately, we carry this inexpensive medication in our office, which is convenient for our patients with Strep Throat.
I live in Detroit, Am I more likely to get the flu or the coronavirus?
You are much more likely to get the flu than the coronavirus if you’re living in the United States.
As of 02/21/2020, there have been 34 documented cases of the Coronavirus in the United States.
Now compare that to the flu or the influenza virus. According to the Centers for Disease Control and Prevention, there have been:
29,000,000 to 41,000,000 flu illnesses
13,000,000 to 19,000,000 flu medical visits
280,000 to 500,000 flu hospitalizations
16,000 to 41,000 flu deaths
We know that the Coronavirus is scary because it’s new and different, and coming from a foreign country. However, the best thing that you can do to prevent getting sick this year is to wash your hands, cover your cough, don’t share drinks or eating utensils, stay home from work when you’re sick so you don’t infect other people, and get your darn flu shot.
Thanks for reading and thanks for watching
-Drs. Paul Thomas MD and Raquel Orlich DO of Plum Health DPC
Emerging Leaders Connect at Michigan Association of CPAs Event
Last week, I was invited as a speaker/panelist at the Michigan Association of CPAs event in Midtown Detroit. The panel focused on entrepreneurship and working with folks who are solo entrepreneurs and self-employed individuals. Many accountants and certified public accountants (CPAs) in Detroit and Metro Detroit are self-employed.
Additionally, many freelancers and self-employed individuals make more than the cutoff point for Medicaid in the State of Michigan (around $17,000) but not enough money to comfortably afford private health insurance. Or, self-employed individuals may not want to spend so much money on health insurance, and rather invest that money back into their businesses.
We take care of many folks in this situation - people are looking for alternative ways to manage their personal health and well-being, and many people are choosing direct primary care services like our Plum Health DPC service as a stand-alone service or as an add-on service to their health insurance plan or catastrophic coverage plan.
This was a great event and brought together many interesting accounting professionals. A big thank you to Matthew Kidd and the Michigan Association of CPAs for the invitation.
Further, it was a pleasure to share the stage with Andrew Dickow, the Managing Director at Greenwich Capital Group. He is an enthusiastic and engaging speaker, and he brought a ton of insights to the table regarding entrepreneurship, investment, and the food and beverage industry in Detroit and beyond.
-Dr. Paul Thomas with Plum Health DPC
We had a great time with the Michigan Association of CPAs Event, called Emerging Leaders Connect. It was a pleasure to speak with Matthew Kidd and Andrew Dickow regarding entrepreneurship in Detroit.
Photos courtesy of:
Kelly Dzierzawski | Video & Creative Services Senior Manager | Michigan Association of CPAs
Dr. Paul Thomas Featured on the Soul of Enterprise Podcast
This month, Dr. Paul Thomas was featured on the Soul of Enterprise Podcast and we had a great conversation around the Direct Primary Care Model and how it can benefit individuals, small businesses, communities, and the nation as a whole. It was great being interviewed by Ed and Ron - they brought a high level of professionalism and integrity to the conversation with some excellent questions around the practice and the DPC model. Enjoy!
WHAT HAPPENS WHEN A SMART DOCTOR RECOGNIZES THAT THERE IS A BETTER WAY?
Is it possible for family physician to operate under a subscription-based business model, priced below what you pay for your mobile phone service? What about services not covered by the subscription? Could those be priced with full certainty and transparency?
For episode 269, we had the pleasure of interviewing Dr. Paul Thomas, founder of Plum Health DPC. Dr. Paul Thomas is a board-certified family medicine physician practicing in Corktown, Detroit. His practice is Plum Health DPC, a Direct Primary Care service that is the first of its kind in Detroit and Wayne County. His mission is to deliver affordable, accessible health care services in Detroit and beyond. He has been featured on WDIV-TV Channel 4, WXYZ Channel 7, Crain's Detroit Business and CBS Radio. He has been a speaker at TEDxDetroit. He is a graduate of Wayne State University School of Medicine and now a Clinical Assistant Professor. Finally, he is an author of the book Direct Primary Care: The Cure for Our Broken Healthcare System.
Below are show notes and questions we asked our guest. Use these to help guide you along when listening to the podcast (embedded above).
Ed’s Questions
What is Direct Primary Care?
Based on an interview I saw you do, there’s no wait time for patients?
Why did you go this route—Direct Primary Care?
You were burned out in your residency. What was the moment that you said I can’t do what most people are signing up to do?
Most time patients do get with their doctors is spent with the doctor typing and facing a screen.
What are some of things that are covered in your clinic?
What you are capable of doing in your practice is probably 80-90% of what a healthy patient would need in a given year?
It would cost me personally about $840 in your practice. If you’re so cheap, why is healthcare so expensive?
It’s said America pays more than the average OECD country, but there’s no price transparency in the system, which inflates those prices, correct?
What are some of the barriers you see that are still in the way of physicians getting into DPC and patients being able to access DPC?
When you did start, did you consider other pricing models? Yours is based on age, but did you consider, for example, response times, or different services you would include and exclude?
Do you have any jumpers, and by that I mean people who pay for a month and then leave, then come back six months later?
You’re now also offering rates to small businesses in your area?
And the companies pay your membership as part of the employees benefit package?
You believe that patients should also have a catastrophic health insurance plan?
We don’t expect our auto insurance to pay for gasoline but we do expect our health insurance to pay for a blood test. It’s absurd?
I was struck that in your TedX talk you used the phrase “living my truth,” take us through that, what does that phrase mean to you?
Ron’s Questions
In your book, Direct Primary Care: The Cure for Our Broken Healthcare System, you cite a 2016 study performed by Medscape found 51% of physicians experience burnout. Burnout is defined as a loss of enthusiasm for work, feelings of cynicism, and a low sense of personal accomplishment. You felt this in your residency. How long did it take you to work up to 500 patients?
How did you market your practice, was it social media, word-of-mouth, press. I know you did a Tedx talk.
I know DPC is in the same family of Concierge Medicine, which has the reputation of being just for the elite, which isn’t true. But the DPC prices are usually less than a mobile phone bill.
On the cover of your book there’s a picture of you trying to catch sand through your hands. Can you explain that analogy?
You talk about technology and how there’s too much borrowing from Henry Ford’s assembly line, treating customers like commodities rather than human interaction. It’s not very efficient to sit and listen to your patient read you poetry. It is, however, highly effective. Would you agree with that?
You also talk how the average of GP doctors have 2,400 patients. Do you think this DPC model will alleviate this GP doctor shortage?
You talk about the growth of urgent care centers in the US is a symptom of a failed primary care system.
Do you feel that people who are not licensed could do some of the work now being done by physicians? What’s your view of occupational licensing and how it folds into this model/
You mentioned to Ed that insurance companies try to get as many dollars passing through the hands. They don’t seem to like the concierge or DPC models, not because they compete with actuarial based insurance but because they compete with pre-paid medical care. Did Michigan pass a law that made it clear that DPC is not an insurance product?
Just seems to be like insurance companies would like to block this model. Is that a fair statement?
There’s obviously some education going on with doctors with respect to DPC, but we also need to re-educate patients to see you even when they are healthy, not just when they are sick. Has that been an educational process to get patients to see you even when they don’t have an issue?
We talk a lot about the market share myth, that growth for the sake of the growth is the ideology of the cancer cell, not a sustainable, profitable business. You phrase it in your book as “Value over volume.” You must be asked a lot that healthcare is different than any other product or service we buy, how do you explain to people that it can be priced like other things we buy
Your model is restoring the sacred relationship between the patient and doctor. You’re bringing this back to the days of Marcus Welby.
I’ve read that most calls (82%) are received during normal business hours, that patients don’t abuse your time off. Has that been your experience unless there’s been an emergency?
Tell us about your new venture, www.startupdpc.com.
If you could wave a magic wand to reform healthcare, what would you do? [Price transparency and quality scores was Dr. Paul’s answer].
HOW TO LISTEN TO THE PODCAST:
Apple Podcast: https://podcasts.apple.com/us/podcast/tsoe-dr-paul-thomas-on-what-is-direct-primary-care/id668653849?i=1000459295760
Try saying, “Alexa, play the Sage Advice Podcast” on your Amazon Echo
Google Play: https://play.google.com/music/m/Dnjmmdjwf4wcptom74ttgymbqam
iHeartRadio: https://www.iheart.com/podcast/263-sage-advice-podcast-27588757/episode/tsoe-dr-paul-thomas-on-53897728/
Spotify: https://open.spotify.com/episode/376LlZkEKLMxe8UH9e8N4J
SoundCloud: https://soundcloud.com/sagena-47293133/tsoe-dr-paul-thomas-on-what-is
PlayerFM: https://player.fm/series/sage-advice-podcast/tsoe-dr-paul-thomas-on-what-is-direct-primary-care
Direct download: http://traffic.libsyn.com/sagena/TLS-TSOE-PaulThomas.mp3
Permalink: http://sageadvicepodcast.com/tsoe-paulthomas
Better Ways to Spend Time and Money on Cyber Monday
There are better ways to spend your time and money during Cyber Monday, I’ll list a few of them here:
invest money into a retirement account, like a Roth IRA or a 401K or 403B plan
put a little extra money into your mortgage, or if you have an auto loan, pay a little extra on your auto loan
invest into a child’s education fund
visit an elderly relative or a neighbor, bonus points if you bring them some nutritious food
go to the gym and have a good work out, bonus points if you go with a friend or a partner/spouse/significant other
take time to make a healthy meal at home
schedule an appointment with your doctor
schedule an appointment with your dentist
check your tires before it snows again
your tread can wear down over time, and sometimes the cold weather can cause deflation
make a donation to a charity
volunteer at a local service organization
if you choose to shop, shop at a local small business and get to know the people that work there and the business owner
write a thank you note to whoever hosted you for Thanksgiving Dinner or a Thanksgiving-related event
meditate
be grateful for what you already have
I know that people can overspend during the Holidays, and I’ve read that people can go into about $1,000 in debt due to holiday spending, but there are better ways to spend your time and money on Cyber Monday. You can invest into yourself and into your retirement accounts, invest into your children’s education funds, take time to exercise and eat healthy foods, and visit and spend time with elderly folks in your life and in your community.
Thanks for reading and have a great day,
-Dr. Paul Thomas
Daily Detroit Covers the Plum Health Move to Corktown
Daily Detroit, shares what to know and where to go in Southeast Michigan in a 15-20 minute, local podcast. They recently covered our move from Southwest Detroit to our new location in Corktown Detroit. Here’s what we discuss:
The move into our new 1,700 Square Foot office in Corktown, at the Corner, which is the historic former site of Tiger Stadium. This is the corner of Michigan and Trumbull, and our address is 1600 Michigan Ave, Suite 125, Detroit MI 48216
We’re a Direct Primary Care practice in Detroit, and we provide Family Medicine services through a membership model for health care. Our members pay $10 each month for children, and our adult memberships start at $49 per month. With the membership, our patients can see us anytime they need to without a copay.
Dr. Raquel Orlich started with our practice in July 2019. She’s an Osteopathic Physician who studied at Michigan State University and was the Chief Resident in Family Medicine at Ascension Macomb.
Why did we move? We moved because we outgrew our original space in Southwest Detroit. We had also won some grant money through the Motor City Match program and the Detroit Demo Day that we needed to use towards our build out of a new office.
Why this specific location? We moved to the Corner because it’s very close to our original location. Our new spot in Corktown is only 1.1 miles away from our old spot in Southwest Detroit. Importantly, this allows us to continue serving all of our original members.
What have we learned since starting this business? If you’ve ever started a business, you know that it’s not the decisions, it’s the decisiveness. This was something that was difficult to learn as a Physician because Doctors are trained to over-analyze problems and leave no stone unturned. I still use that part of my brain when taking care of patients, but I have to turn that part of my brain off when I think about challenges in our business.
How can people get involved? You can enroll on our website, here. Or you can give us a call at 313.444.5630. Finally, you can stop by at our new office - 1620 Michigan Ave Ste 125, Detroit MI 48216.
Listen to the episode on Daily Detroit’s YouTube Channel (below). Our segment starts at the 4:28 mark.
If you like Plum Health, and if you like YouTube, you’ll love our Plum Health YouTube Channel!
Thanks for reading and watching and have a marvelous day - Dr. Paul Thomas and Dr. Raquel Orlich
How to Quit Drinking Alcohol in Detroit
The holidays are just around the corner. It’s that time of year we catch up with good friends and loved ones. As we are celebrating, it is important that we safely enjoy our alcoholic beverages. It is also imperative to be transparent with your doctor about the amount of your alcohol consumption as we will discuss more below, can greatly impact your physical health causing chronic ailments like heart disease, high blood pressure, and liver disease. Excessive alcohol use can also be associated with mental health concerns such as depression and anxiety.
What does it mean to be above the legal limit for drinking?
According to the CDC, all states in the United States have adopted a blood alcohol content percentage (BAC) 0.08% as the legal limit for operating a motor vehicle for drivers aged 21 years or older. However, drivers younger than 21 are not allowed to operate a motor vehicle with any level of alcohol in their system.
Legal limits are measured using either a blood alcohol test or a breathalyzer.
Legal limits are typically defined by state law, and may vary according to individual characteristics, such as age and occupation.
What is one “drink” according to the CDC?
12-ounces of beer (5% alcohol content).
8-ounces of malt liquor (7% alcohol content).
5-ounces of wine (12% alcohol content).
1.5-ounces (1 shot glass) of liquor (e.g., gin, rum, vodka, whiskey).
What are the current recommendations for alcohol use?
With the holidays approaching, it is important to drink alcohol in moderation. This means 1 drink per day for women, and 2 drinks per day for men. These recommendations should adhere to the one “drink” standard described above. This means that wine glasses should not be filled to the brim! It is always important to keep in mind that with certain medications interact with alcohol use, including sleeping pills, muscle relaxers or other sedative medications that may make you drowsy. Always be sure to consult your physician and check your prescription bottle for recommendations in regards to alcohol consumption.
Guidelines for Excessive Drinking
According to the CDC, binge drinking includes 4 alcoholic beverages for women, or 5 for men, in a two-hour period. Heavy drinking is considered 8+ drinks per week for women, or 15+ drinks per week for men. Any drinking by a pregnant women or individual under the age of 21 is considered excessive.
What are signs of Alcohol Use Disorder?
Some of the signs and symptoms of alcohol use disorder could include:
Inability to limit drinking.
Continuing to drink despite personal or professional problems.
Needing to drink more to get the same effect.
Wanting a drink so badly you can’t think of anything else.
Health Risks of Alcohol Use
According to the CDC, there are short-term and long-term health risks associated with heavy alcohol use.
Short-Term Health Risks
Excessive alcohol use has immediate effects that increase the risk of many harmful health conditions. These are most often the result of binge drinking and include the following:
Injuries, car crashes, falls, drowning, and burns.
Violence, including homicide, suicide, sexual assault, and intimate partner violence.
Alcohol poisoning, a medical emergency that results from high blood alcohol levels.
Risky sexual behaviors, including unprotected sex or sex with multiple partners. These behaviors can result in unintended pregnancy or sexually transmitted diseases, including HIV.
Miscarriage and stillbirth or fetal alcohol syndrome disorder among pregnant women.
Long-Term Health Risks
Over time, excessive alcohol use can lead to the development of chronic diseases and other serious problems including:
High blood pressure, heart disease, stroke, liver disease, and digestive problems.
Cancer of the breast, mouth, throat, esophagus, liver, and colon.
Learning and memory problems, including dementia and poor school performance.
Mental health problems, including depression and anxiety.
Social problems, including lost productivity, family problems, and unemployment.
Alcohol dependence, or alcoholism.
Signs of Alcohol Withdrawal
After discontinuing alcohol use, within the first 2-4 days days it is possible to have several symptoms including, shakiness, sweating, loss of appetite, nausea, vomiting, headaches and a fast heart rate (also known as tachycardia). More serious symptoms include delirium tremens (DT), seizures and death. Any withdrawal from alcohol should be monitored by your healthcare provider as these symptoms may occur.
Resources for Alcohol Use
Substance Abuse and mental health services’ (SAMHSA) National Helpline number, open 24/7 365 days, 1-800-662-HELP (4357)
For more information on how you can safely consume alcohol this winter, please visit the CDC.
How To Quit Drinking Alcohol in Detroit
If you need help with quitting drinking alcohol, we’re happy to help. We can direct you to the best resources available for alcohol cessation, and we can treat alcoholism in our office. The Sinclair Method is a reasonable treatment option in some cases and it involves taking Naltrexone one hour prior to alcohol consumption. There are also local Alcoholics Anonymous meetings and other support groups that you can attend to help you reduce or eliminate your alcohol consumption.
Thanks for reading and have a great day,
-Dr. Paul Thomas and Dr. Raquel Orlich
How to get a Pap Test in Detroit?
Affordable Pap Tests Available at Plum Health
Ladies - it’s time that we talk about Women’s Health! An important aspect of routine follow-up with your primary care physician is to discuss screening tests for preventable diseases such as heart disease, high blood pressure, and diabetes. Additionally, it is important to talk to your doctor about cancer screening tests that may be appropriate for you such as for screening for breast, colon, and cervical cancer.
Many of us know that mammograms are great screening tests to look for breast cancer --Did you know October is Breast Cancer Awareness month? Additionally, a colonoscopy is used (a procedure that uses a camera to look in your colon) for colon cancer screening. However, not as many of us know why our doctors stress the importance of cervical cancer screening and what a pap smear is.
Below we will explain the basics: What is a cervix? What causes cervical cancer? What is HPV? What is a Pap test? When should I get one?
What is a cervix?
The cervix is a muscle at the lowest part of the uterus. It meets with the deepest part of the vaginal canal. There is also a small opening in the center of the cervix called the cervical canal that connects the vagina and the uterus. This opening can open and close at different times --- It opens slightly during your period and fully during childbirth. But it also protects against infections from entering into the uterus. Amazing right?
Cervical cancer and Human Papillomavirus (HPV)
Unfortunately, this opening of the cervix can become infected by a very common virus called Human Papillomavirus (HPV). In most cases, the infection will clear on its own, however if the infection does not clear on its own, it can pose a risk of developing cervical cancer. According to the Centers for Disease Control and Prevention (CDC),12,845 new cervical cancer cases were diagnosed in 2015 and 4,175 deaths were caused by cervical cancer in 2015.
More about Human Papillomavirus (HPV) and how is it transmitted?
According to the Centers for Disease Control and Prevention (CDC), HPV infections are so common that nearly all men and women will get at least one type of HPV at some point in their lives. Nearly 80 million Americans are currently infected with some type of HPV. About 14 million Americans, including teens, become infected each year.
HPV is spread through intimate skin-to-skin contact. You can also get HPV by having vaginal, anal, or oral sex with someone who has the virus. There are many types or strains of this virus. Some of the strains can cause warts on the hands and feet and others can infect tissues of the genital region which can cause warts in that region as well BUT can also be associated with some cancers of genital region (i.e. vagina, penis, and anus) and of the head and neck.
What has been done to help prevent HPV infections?
At this time, the CDC recommends that all boys and girls start vaccination against HPV infection that can be started as early as age 9 through 26 years of age. As of October 2018, the US Food and Drug Administration (FDA) has approved the vaccination for men and women through 45 years of age with Gardasil 9 (common name brand for one of the vaccines). For the HPV vaccine to be most effective, the series should be given prior to exposure to HPV.
Dr. Paul Thomas and Dr. Raquel Orlich of Plum Health DPC discuss cervical cancer screening at their office in Detroit, Michigan.
How can your doctor screen for cancer and precancers of the cervix?
If you are between the ages of 21 and 65 years of age, your doctor will start screening you for cervical cancer. The screening test is called the Papanicolaou test aka the “Pap test or Pap smear”. During a Pap smear, your doctor will need to visualize your cervix with a small utensil called a vaginal speculum. With a small brush, he or she will gently scrape the cervix to collect a sample of the cells in the opening of the cervix. This procedure takes less than 5 minutes and most women report it to be painless or may have minimal discomfort. The sample is then sent to the lab for review.
According to the CDC, decline in cervical cancer cases and deaths in the past 40 years correlated with Pap testing and detection and treatment of cervical precancerous lesions. The majority of cervical cancers (50% to 64%) occur in women who were rarely or never screened.
The screening guidelines recommend that women between the ages of 21 and 29 years old should have routine screening every 3 years.
The screening guidelines recommend that women between the ages of 30 and 65 year old have two options for routine screening --
Have a Pap test every 3 years or
Have a Pap test with an HPV test every 5 years.
*However, if your results are abnormal, you will discuss with your doctor when you should return for a follow-up Pap test or need additional testing.
Luckily, cervical cancers usually take years to develop. If you’re getting screened regularly (every 3 or 5 years), you are extremely unlikely to develop cervical cancer. Let’s take control of our feminine health!
You can visit the CDC for more information on the Pap test and HPV
What does the Pap test NOT test for?
The Pap test does not test for sexually transmitted infections such as chlamydia, gonorrhea, herpes simplex, syphilis, or HIV.
How much does it cost to have a Pap test?
Depending on your insurance plan, Pap testing may be covered as a preventive service. If you are underinsured or uninsured, the test may be costly.
If you are a member of Plum Health DPC, we are able to provide affordable prices for many screening tests including Pap tests. The price of our Pap test is $30 to $60
How can I sign up for an appointment for a pap smear?
To make an appointment with Dr. Raquel or Dr. Paul, head over to our scheduling link and select her or him as your doctor. After you submit the information, Dr. Raquel will reach out and offer appointment times.
Thank you for reading and have a great day,
-Dr. Paul Thomas and Dr. Raquel Orlich with Plum Health DPC
Plum Health at the Detroit Men's Health Event
This week, we were at Ford Field for the Men's Health event. The event was really fun and really well organized. There were stations to have blood pressure checks, EKGs, Vision Screening, Vein Examinations, Skin Examinations to screen for Cancer, and several other tables with information about follow up care and the like.
Raquel Orlich, DO and Paul Thomas, MD of Plum Health DPC at the Ford Field Men’s Health Event.
We were happy to be invited and we met with several Detroit men and women in need of excellent primary care services. There were also some fun moments - they had a giant colon set up to promote colorectal cancer screening tests, like a colonoscopy. Also, we were able to go onto the playing field of the Detroit Lions, throw around a football and kick a few field goals! This was really cool and a nice perk of volunteering at the event.
Finally, if you’re looking for high-quality primary care services for you and your family, we’d be happy to help you with this sort of care. You see, at this type of event, conditions like high blood pressure and diabetes can be diagnosed, but the most important part is the follow up care after the diagnosis to make sure the condition is treated appropriately, well-managed, and ideally reversed with the right diet and lifestyle modifications.
Thanks for reading and have a great day,
-Dr. Paul Thomas and Dr. Raquel Orlich of Plum Health DPC
Detroit Family Medicine Office Offers Affordable In-Office Procedures
Detroit Family Medicine Office Offers Affordable In-Office Procedures
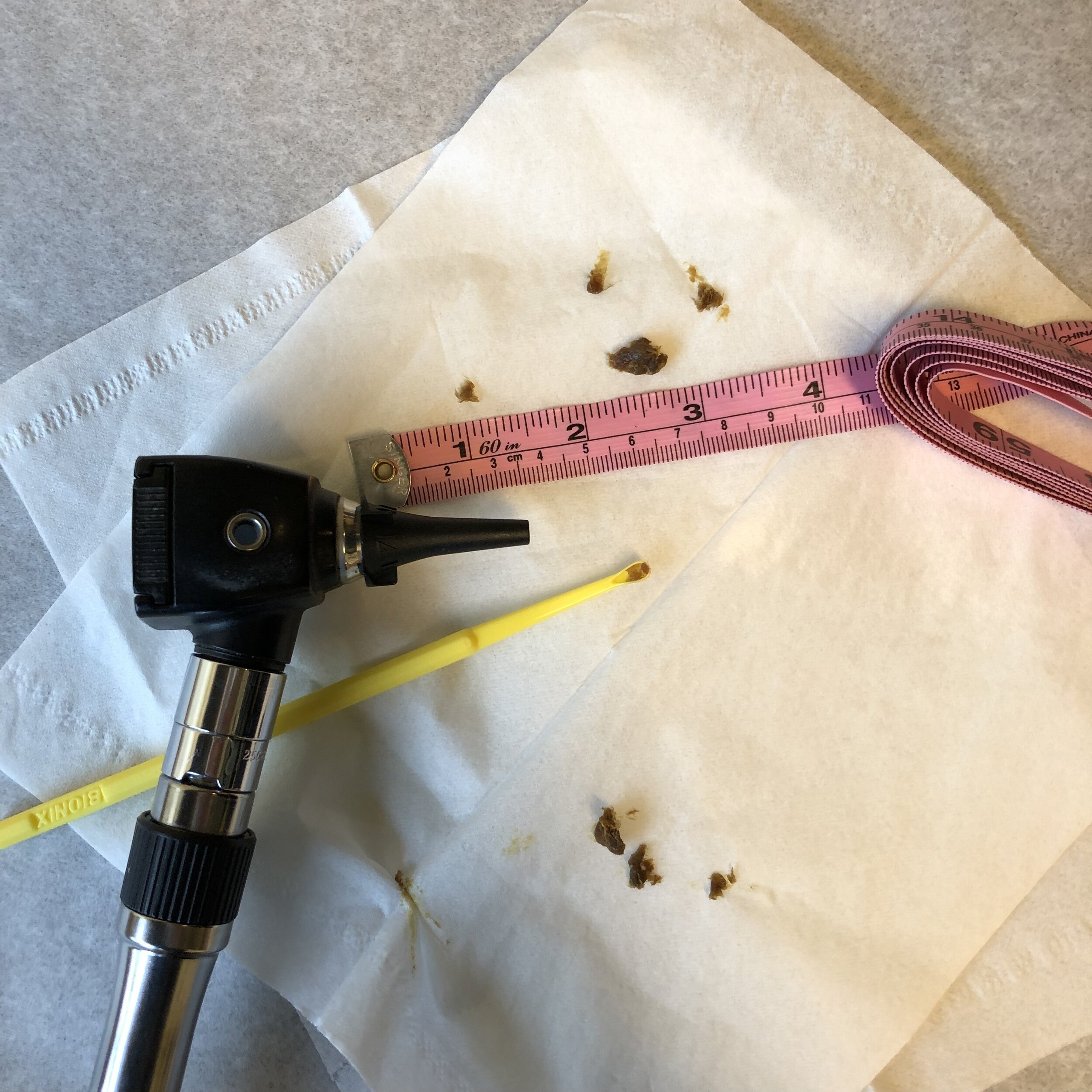
The beauty of Family Medicine Practice is it can be a one stop shop for you and your medical care. Family doctors can usually take care of 80-90% of your medical needs and that includes medical procedures. Family doctors are trained to perform a wide variety of procedures that can be offered in the office. This can help you save time and money from sending you to a specialist. At Plum Health, we love taking care of procedures for our patients, these can range from Pap tests to biopsies, from toenail removal to earwax removal, from abscess drainage to lipoma removals.
Our patient cut his hand aka had a laceration, and we were able to sew up the cut (suture the wound) about 20 minutes after the incident happened. This can ensure that healing is optimal and scar tissue is minimal.
List of Common In-Office Procedures Performed by Family Medicine Doctors
Some of the procedures that Family medicine physicians can perform are listed below.
Procedures that can be performed by your Family Doctor
Wound repair (sewing up small to medium sized cuts)
Abscess and cyst drainage
Skin biopsy of moles
Steroid Injection of joints and trigger points
Electrocardiogram (EKG)
Pulmonary Function Test
Pap smear
IUD (intrauterine device) removal
Ingrown toenail removal
Wart removal
Foreign body removal
Osteopathic Manipulative Medicine
Cerumen Disimpaction (ear wax removal)
With a flick of the wrist we can remove a significant amount of cerumen (ear wax) that may be impairing your hearing. There is no charge for this cerumen disimpaction procedure in our office.
Unfortunately, some of these procedures can be very costly depending on your insurance plan or lack thereof. A major reason for the expense of procedures vary from your insurance deductible plan and insurance coverage. Usually, the doctor’s offices will charge the insurance companies for the procedure. This inflates the cost.
For example, a typical charge for a sebaceous cyst removal might be $175 - $350. That service is $20 in our office. A skin biopsy can cost anywhere from $150 - $1,000 and an IUD removal can cost $150 - $250. For these procedures, we typically charge about $20 or the cost of the supplies that we use to perform these procedures.
Why are Common In-House Procedures Less Expensive at Plum Health?
At Plum Health DPC, we do not use or bill insurance for your medical care. Our membership plan does include performance of some procedures which helps cut many costs. We may be subject to charge for utensils and medications used during the procedure which is also offered at a discounted price.
Because the patients in our practice pay a monthly membership fee, we can lower the cost of procedures. Instead of charging you or your insurance company $100 or $500 for a procedure, we ask that you pay for the cost of the supplies that we use.
How to Schedule an Appointment to have a Procedure at our Detroit office
To make an appointment with Dr. Raquel Orlich or Dr. Paul Thomas, head over to our scheduling link. After you submit the information, Dr. Raquel or Dr. Paul will reach out and offer appointment times.
Thank you for reading and have a great day,
-Dr. Paul Thomas and Dr. Raquel Orlich
How to Get a Flu Shot in Detroit
How to Get a Flu Shot in Detroit
Flu season is just around the corner and according to the Centers for Disease Control (CDC), “During the 2017–2018 influenza season there was an estimated 959,000 hospitalizations and 79,400 deaths due to complications of influenza infection.
So nearly 1 million hospitalizations and close to eighty thousand deaths due to a vaccine preventable illness! This is why we advocate for getting a Flu Shot before the start of the Flu Season - we want to prevent people from going to the hospital and potentially dying from the flu aka influenza.
How Effective is the Flu Shot aka Influenza Vaccine?
The CDC conducts studies each year to determine how well the influenza (flu) vaccine protects against flu illness. While vaccine effectiveness can vary, recent studies show that flu vaccination reduces the risk of flu illness by between 40% and 60% among the overall population during seasons when most circulating flu viruses are well-matched to the flu vaccine.
So, if you get the flu shot, and the vaccine is well-matched to the circulating virus, you can reduce your risk of getting the Flu by about half - that’s great!
Influenza Vaccine for the 2019 - 2020 season given to one of our patients at Plum Health DPC in Detroit, MI.
How Can the Flu Shot Help Me?
There are many reasons to get a flu vaccine each year. Below is a summary of the benefits of flu vaccination:
Flu vaccination can keep you from getting sick with flu.
Flu vaccination can reduce the risk of flu-associated hospitalization for children, working age adults, and older adults.
Flu vaccination helps prevent serious medical events associated with some chronic conditions such as heart disease, diabetes, and chronic lung disease.
Vaccination helps protect women during and after pregnancy.
Flu vaccine can be life-saving in children.
Flu vaccination has been shown in several studies to reduce severity of illness in people who get vaccinated but still get sick.
Getting vaccinated yourself may also protect people around you, including those who are more vulnerable to serious flu illness, like babies and young children, older people, and people with certain chronic health conditions.
So, if you’re a parent with young children, by getting the Flu Shot, you can help protect your kids. If you’re someone with many chronic diseases like diabetes or heart failure, getting the flu shot can reduce your risk of these diseases worsening if you were to be infected with the flu.
What are Flu Symptoms? What Should I Look Out For?
Flu Symptoms have a broad range, but typically people come to the doctor with the following concerns:
Fever* or feeling feverish/chills
Cough
Sore throat
Runny or stuffy nose
Muscle or body aches
Headaches
Fatigue (tiredness)
Some people may have vomiting and diarrhea, though this is more common in children than adults.
As a doctor treating folks with the flu, there’s something called the pajama sign - if you don’t have the energy to shower and get dressed into regular clothes, and you have some of the above symptoms, it’s more likely that you have the flu. Seriously - I’ve had people compare getting the flu to being hit by a truck - getting an illness as severe as the flu can feel like all of your energy has been taken away.
How Is the Flu Virus Spread?
Most experts believe that flu viruses spread mainly by tiny droplets made when people with flu cough, sneeze or talk. These droplets can land in the mouths or noses of people who are nearby. Less often, a person might get the flu by touching a surface or object that has flu virus on it and then touching their own mouth, nose or possibly their eyes.
To rephrase, someone might cough and they might have tiny droplets fly out of their mouth and land on things that you touch, like door handles, shopping cart handles, tables at a restaurant, etc… That’s why it’s so important that you wash your hands before touching your own nose and mouth and before eating. If you are sick, it’s also very important to wash your hands after coughing and sneezing. You can help lessen the spread of the flu virus by washing your hands often during cold and flu season.
For more information, visit the CDC for the most up-to-date information on the flu.
How to Get the Flu Shot in Detroit
Protect yourself and your family (and friends and co-workers) from the flu this year! To make an appointment with Dr. Raquel, head over to our scheduling link and select her as your doctor. After you submit the information, Dr. Raquel will reach out and offer appointment times.
Thank you for reading and have a great day,
-Dr. Paul Thomas and Dr. Raquel Orlich with Plum Health DPC
Influenza Vaccine instructions for the 2019 - 2020 Vaccine Season including ingredients in the vaccine.
Helping Other Detroit Entrepreneurs with their Businesses
Last week, I was invited to participate in a Business Coaching Program with the BUILD Institute and Samuel Adams. It was held at the Jam Handy. BUILD Institute had coordinated for roughly 50 business coaches and 100 small business owners/start up founders to come through for business coaching.
April Boyle runs the BUILD Institute and they focus on helping entrepreneurs start businesses. They give entrepreneurs a set of tools to get started, by focusing on a curriculum with sessions regarding accounting, finance, marketing, branding, customer acquisition, leveraging capital, etc… This where I started my entrepreneurial journey, so I’m excited to be a part of this group!
It was a fun event with a ton of energy in the room - lots of great ideas and exciting new business ventures. It’s great to see a strong entrepreneurial ecosystem in Detroit and it was fun to be a part of this event. Here’s some pics!
Dr. Paul Thomas of Plum Health DPC volunteering at the Build Institute’s Business Mentorship night at the Jam Handy in Detroit, Michigan.
Group Pics:
A funny story about the above photo session. I was in the back and obstructed, so I took a big jump and seemed to time it pretty well! You can see me leaping in the back.
Have a great day - Dr. Paul