Plum Health Blog
Plum Health with the Black Health Academy
Last month, we had a great visit from and interview with Lisa A. Smith with the Black Health Academy. We first met during a small business course with the Build Institute in Detroit, and it was great getting back together for this interview! She has a passion for health and wellness and helping people reach their full potential. Here's how she tells her story on her webpage:
Lisa A. Smith, MBA, is the founder of Professionally Fit INC and The Black Health Academy. She began her own weight loss journey in 2012 at 190 lbs. She fell in love with fitness, nutrition and self-development, lost over 60 lbs and gained a bottomless amount of confidence. It wasn't until she gained confidence in her physical health that she was able to gain confidence in her career. With her new found confidence she launched Professionally Fit in July of 2015. Professionally Fit is an executive coaching platform which provides both the customization and accountability necessary for high performing entrepreneurs and executives to achieve their health and wellness goals from anywhere in the world.
Health disparities in detroit
Our conversation focused on health and wellness in the black community. There are almost unbelievable health disparities between white Americans and black Americans, and we discuss some of these differences during our interview. Lisa also highlights these disparities on her website:
Here are the facts:
- 47.8% of African Americans are considered overweight or obese
- African Americans are 20% less likely to be treated for depression
- 13.6% of African Americans have fair to poor health
- 40.9% of black men over the age of 20 have high blood pressure
- Heart disease, cancer and stroke are the leading causes of death in the black community
Topics covered during our masterclass
During our Masterclass, we discuss these health disparities, what inspired me to become a physician, the community-focused efforts at Wayne State University School of Medicine, why other physicians might not practice in a more community service-oriented way, what Plum Health is, how we manage the volume of patients in our practice, our range of services or scope of practice, the type of feedback that we've been getting from our members, trends in African American health, on not making assumptions about people's health and meeting people where they're at, and on making lifestyle recommendations versus taking medications.
I really loved this interview with Lisa A Smith - it was like siting down with an old friend. If you want to learn more about her and what she does, please visit the Black Health Academy or follow her on Facebook.
Thanks for reading and watching, and have a wonderful day!
- Dr. Paul Thomas with Plum Health DPC
PS Follow us on Instagram!
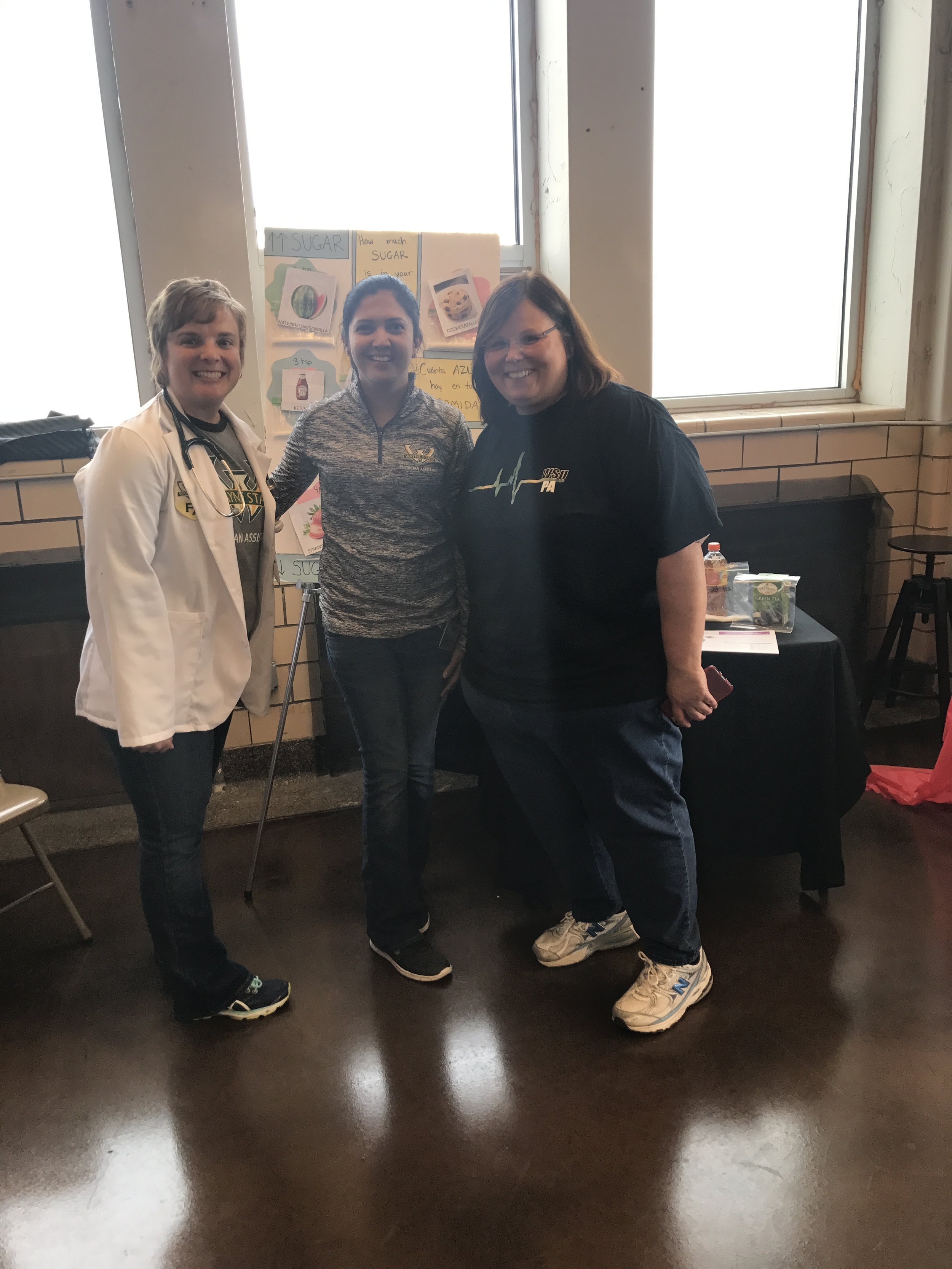
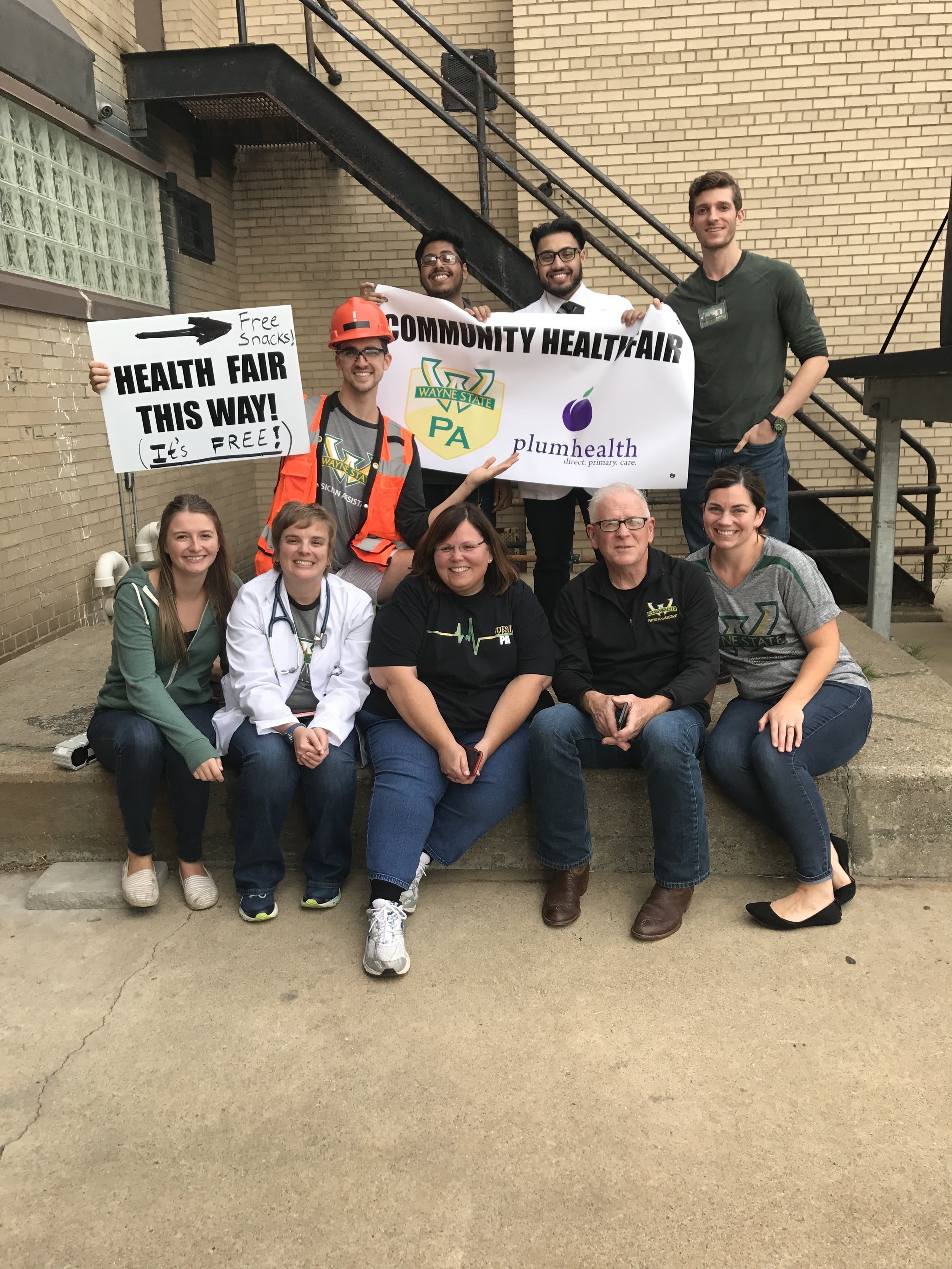
Health Fair with the Wayne State Physicians Assistants
Over the past 6 months I've been hosting and teaching Physician Assistant students from Wayne State University at the Plum Health office. I've also had a few residents rotate through and a few medical students visit the clinic, some from Wayne State and some from University of Michigan.
As Plum Health is the only Direct Primary Care practice in Detroit and Wayne County, and only one of less than ten in the State of Michigan, I find that we attract PA students, medical students, residents, doctors and allied health professionals who are thinking differently about health care and it's delivery, especially in the context of health equity and health disparities.
Anyways, I've loved having these students rotate through Plum Health! They bring a unique perspective, build genuine relationships with our members, and create an atmosphere of teaching and learning in the practice. This last point is important because I practice evidence-based medicine, and having a student helps to keep me up-to-date on the latest recommendations for evidence-based practice.
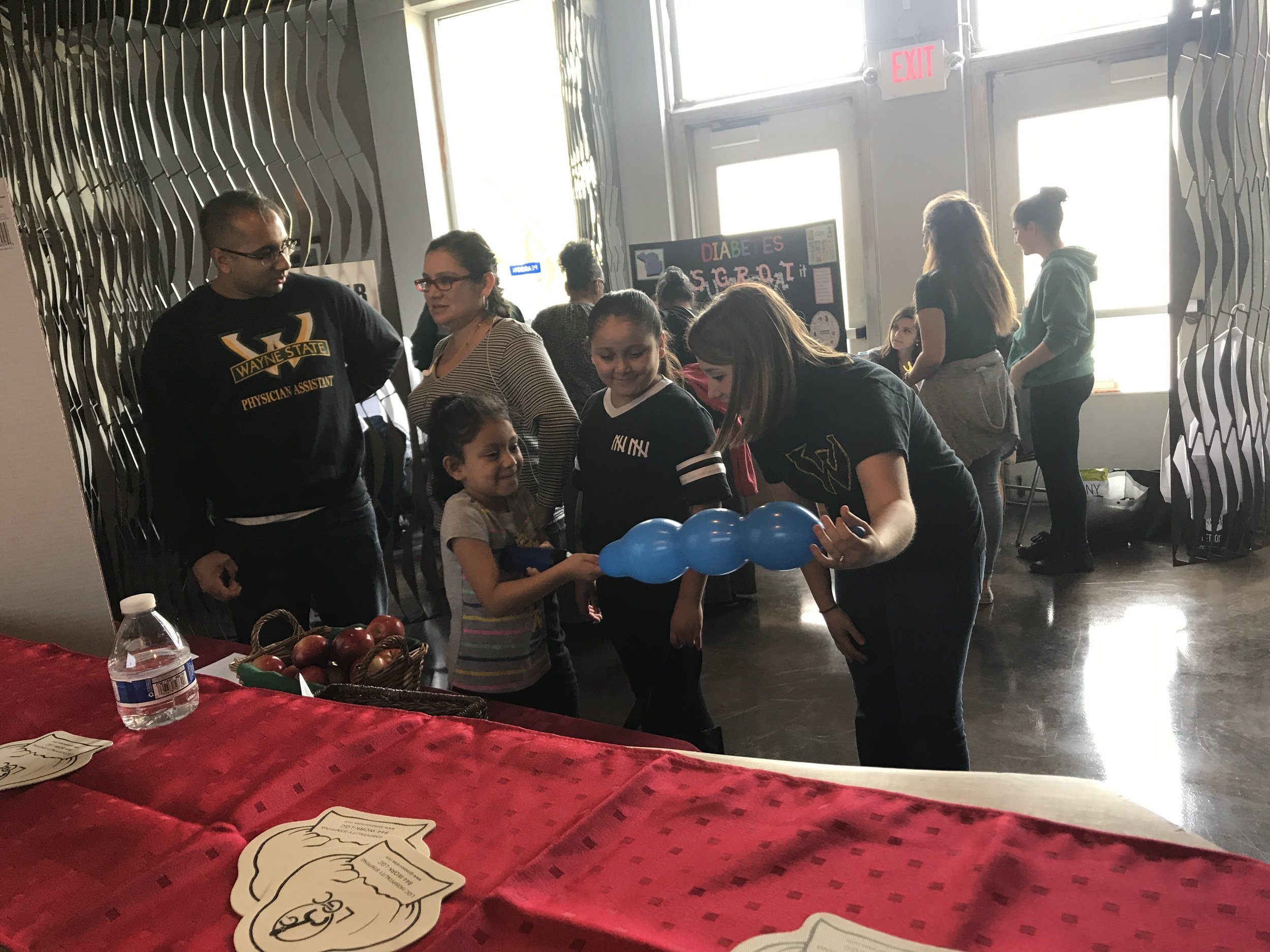
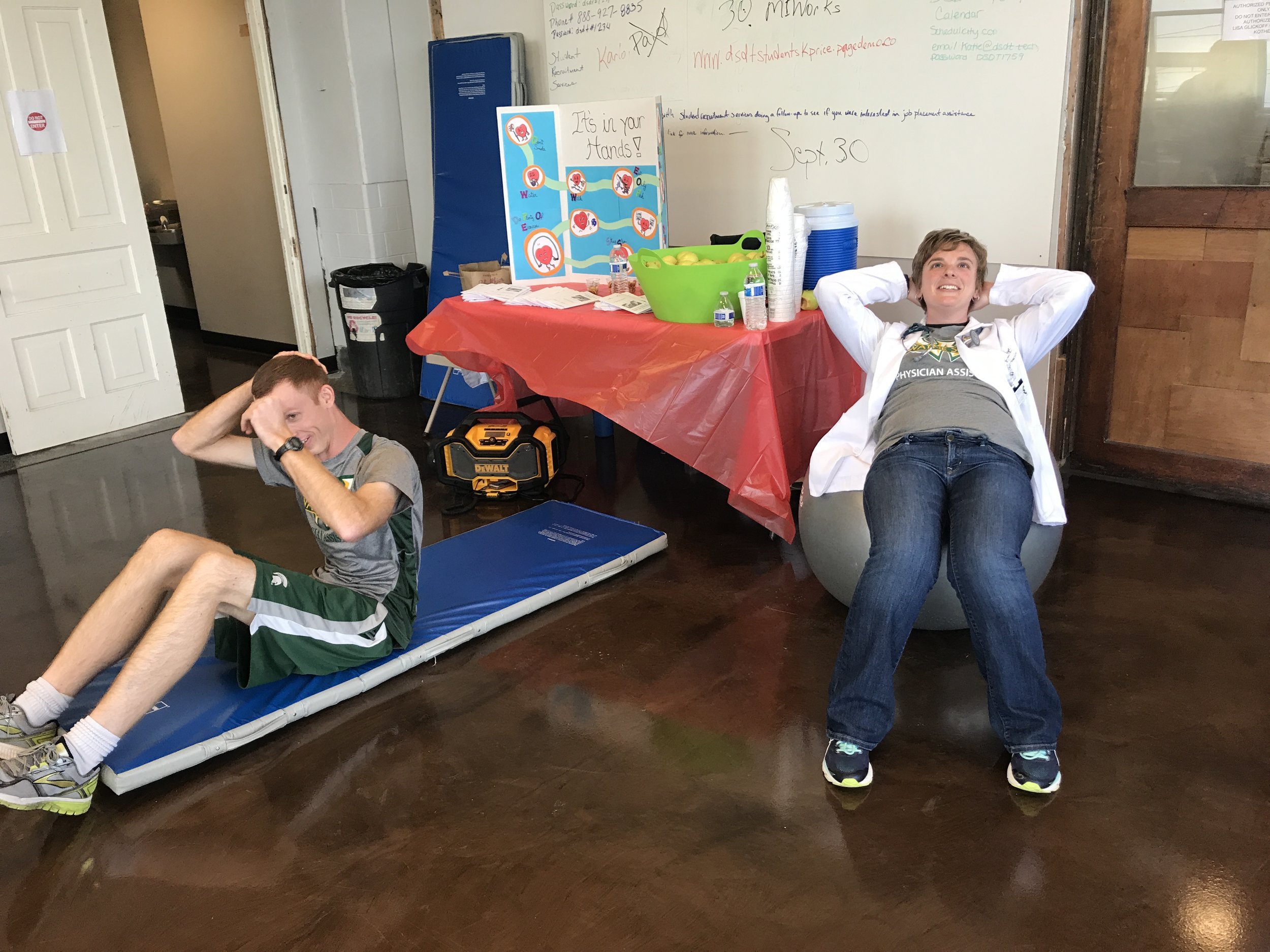
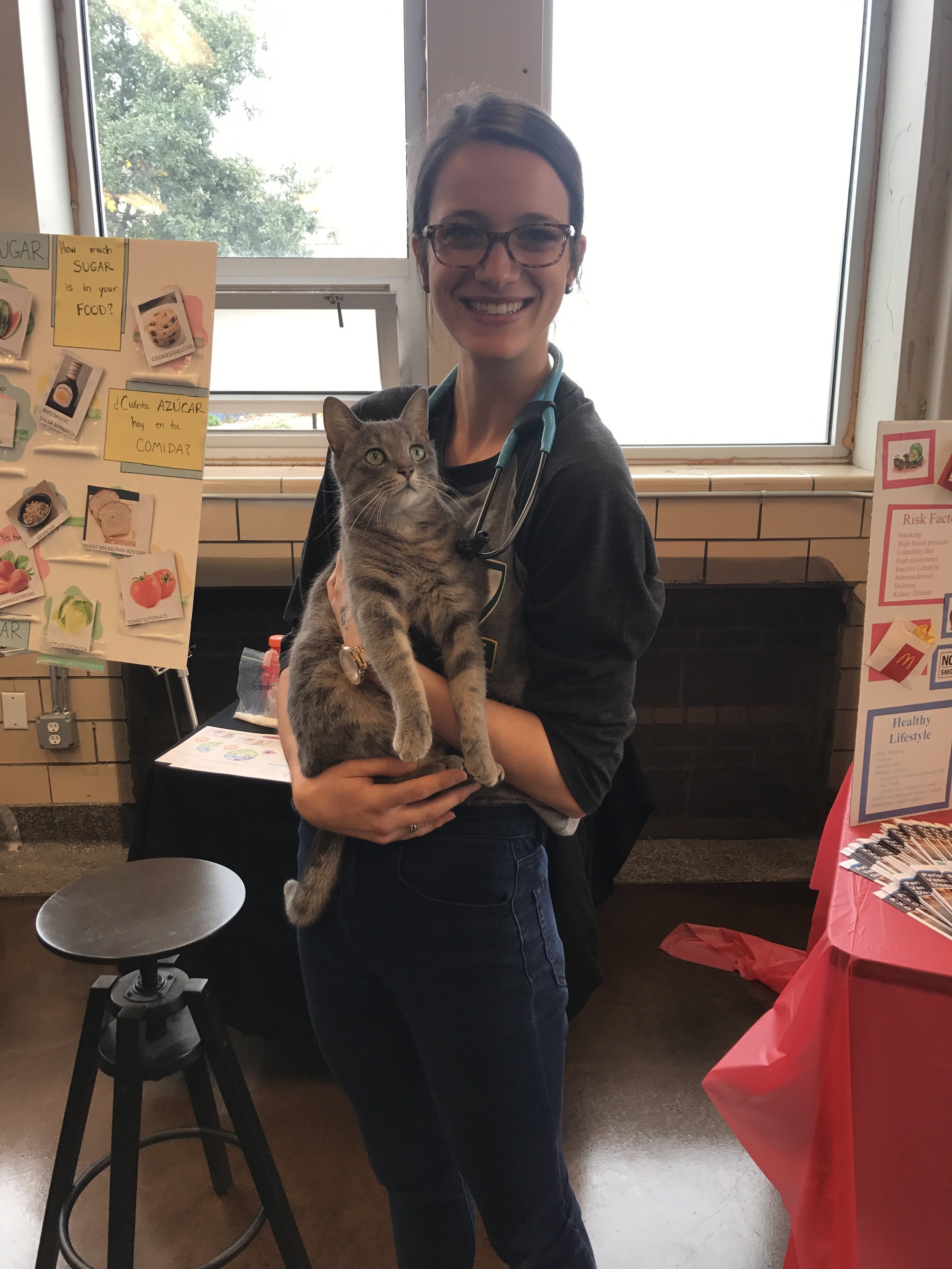
So last weekend, we were able to host a health fair at the Plum Health office. "We" being myself and the Physician Assistant students at Wayne State. Their energy was boundless and they put a great deal of time and effort in creating fun health-focused stations that taught participants about being healthier.
All in all, it was a successful day! We reached out to new people in the community, and gave away free medical care. We caught a case of diabetes that was unknown prior to the fair and helped folks gauge their blood pressure, blood sugar, and cholesterol levels (HDL, LDL, Total Cholesterol and Lipid Panel).
Below are photos from the event! Thanks for reading, and have a great day!
- Dr. Paul Thomas with Plum Health DPC in Detroit, Michigan
Opinion Published in the Detroit News
This week I wrote an opinion piece and it was published by the Detroit News! I'm very excited about getting the word out about the benefits of Primary Care and the work that needs to be done to address the health disparities in our city and in our region. Here's the link. A sincere thank you to Ingrid Jacques for giving me the opportunity to write this.
There are always constraints, with time and with resources, and the article was edited to fit the allotted space in the Sunday paper. So, here is the essay that I wrote in its entirety prior to editing by the News:
If you live in the City of Detroit, you may find yourself driving to the suburbs for your primary care services.
According to top officials in the Detroit Health Department, there are roughly 50 – 100 primary care doctors in Detroit. For a city of 683,000 people, that’s about 1 doctor for every 6,000 – 12,000 residents, which is horribly underserved.
Interestingly, Wayne County as a whole has 1 primary care doctor for every 1,515 residents. But, the supply of doctors is not equitably distributed across communities within Wayne County. Areas like Grosse Pointe and Dearborn have a relative saturation, while cities like Inkster and Detroit remain underserved.
By contrast, Washtenaw County has 1 primary care doctor for every 598 residents and Oakland County has 1 primary care doc for every 655 residents. These are more equitable and desirable ratios.
We need more primary care doctors in our communities. Research has shown that as the number of primary care doctors increases, health outcomes improve and costs decrease.
Data released by the American Academy of Family Physicians reveals that an increase in one primary care doctor per 10,000 people reduces hospital admissions by 5.5%, ER visits by 10.9% and surgeries by 7.2%.
In an era of greater awareness of healthcare expenditures, that’s a lot of bang for your buck.
Unfortunately, the medical system does not incentivize primary care medicine. Specialists like Orthopedists, Cardiologists and Dermatologists are reimbursed at much higher rates than primary care specialists like Family Medicine doctors, General Internal Medicine doctors and Pediatricians.
And the graduating medical student is acutely aware of these discrepancies in pay. The median level of med school debt for the class of 2015 was $183,000 and the total cost may surpass $400,000 if paid over the long term with interest.
As the average student considers an average salary of $443,000 as an Orthopedist or $204,000 as a Pediatrician, choosing primary care medicine becomes economically strenuous.
And for those doctors who choose primary care specialties, primary care offices are often set up in more affluent neighborhoods where the reimbursement levels are higher. These location selection decisions are often out of the hands of individual doctors and dictated by corporate, profit-driven health systems.
This suburbanization of primary care medical services has had a terrible effect for Detroit’s residents. WalletHub recently ranked the City of Detroit as the least healthy major city in the United States, ranking 150 out of 150.
After the WalletHub list was published, the former Health Department Director was quoted in a Detroit News article: “Detroit health chief Dr. Abdul El-Sayed wasn’t surprised with the results, which he blamed partly on the lack of doctor’s offices in neighborhoods, healthy food stores, transportation and safe places to exercise.”
But, there is hope. The longstanding work of free and low cost clinics like CHASS, the Student Run Free Clinic, HUDA, and Joy-Southfield Clinics should be acknowledged. It is also encouraging that the Michigan State University of Osteopathic Medicine Popoff Clinic on Mack Avenue on the East Side is complimenting these stalwarts. Additionally, a Direct Primary Care service, Plum Health DPC, in Southwest Detroit/Corktown is providing another option for Detroit residents.
Finally, as Downtown, Midtown and New Center become more sustainable, primary care services should begin to take hold with potential spill over benefits for adjacent neighborhoods.
Paul Thomas, MD
Family Medicine Doctor with Plum Health DPC
Thank you for reading, and have a wonderful day,
- Paul Thomas, MD
A newspaper clipping from this Sunday's Detroit News about health care and health disparities in the city of Detroit and the potential solutions to address them.
The Importance of Primary Care
Primary care is essential to having a healthy family, healthy community, and a healthy society. You may know a primary care doctor, like your Family Medicine doctor, General Internist, Pediatrician, or Gynecologist. These are the doctors that partner with you to create better health outcomes.
There's been a great deal of research conducted about the benefits of having community doctors or primary care doctors. In an article from the American Academy of Family Physicians, it is noted that "an increase of one primary care doctor per 10,000 people has been shown to result in:
- 5% decrease in outpatient visits
- 5.5% decrease in inpatient admissions
- 10.9% decrease in ER visits
- 7.2% decrease in surgeries"
Further, counties with more primary care doctors have lower healthcare costs and better mortality rates. MLive.com wrote a nice piece about the importance of primary care doctors and they even have a tool so that you can evaluate how many primary care docs are in your community. In Washtenaw County, there's a primary care doctor for every 598 residents. In Cass County, there's a primary care doctor for every 7,463 residents.
Washtenaw County is likely saturated with primary care doctors because it encompasses Ann Arbor and the U of M Health System. From the MLive.com article, "The U.S. Department of Health and Human Services' Health Resources and Services Administration has calculated that Michigan's supply of primary care physicians meet 63.3 percent of the population need." That means about 63% of the state is serviced with enough primary care providers.
Unfortunately, Detroit itself is underserved. There are roughly 50 - 100 primary care doctors in Detroit for roughly 680,000 residents. That's roughly 1 doctor for every 6,000 - 12,000 residents in the City of Detroit.
If you were to look at the data for Wayne County, which includes Detroit, Dearborn, Inkster, the Grosse Pointes, etc..., you would see that there's 1 doctor for every 1,515 people, which is a relatively equitable ratio. However, when you look closer at the distribution of physicians in Wayne County, you will see that several are concentrated in wealthier suburbs like Grosse Pointe and Dearborn. This leaves places like Detroit and Inkster underserved.
The black dots on this map indicate the locations of licensed physicians. While there are a good number of doctor's offices in Wayne County, the distribution of these offices is skewed with a higher concentration of offices in Dearborn and Grosse Pointe than in the City of Detroit itself. This image was a part of a larger presentation given by former Detroit Health Department Director and now Candidate for Governor of Michigan, Abdul El-Sayed. In case you were wondering, the yellow stars indicate pop-up clinics planned by the City of Detroit Health Department to distribute contraceptives.
One of the several reasons why I've started Plum Health in Detroit is to address the health disparities and access to care issues that are currently facing the City. Because we provide our services, medications, labs, and imaging at such an affordable price, we are able to care for people of all socio-economic strata. This allows us to aspire to a more just and equitable health care system, and it starts with excellent primary care.
Finally, I want to inspire high school students, college students, medical students at Wayne State University, and current Family Medicine residents to practice Family Medicine in a Direct Primary Care practice or traditional fee-for-service model in the City. We need excellent primary care doctors for our community to be healthier and to address the health disparities in our city.
Yours in Good Health,
- Paul Thomas, MD
Medical Equity Conference
Yesterday, I attended the Inaugural Health Equity Research Conference at Wayne State University. It was held in the student center and brought together several stakeholders in Detroit. The day began with several excellent presentations from undergraduate students and medical residents, ranging from Sickle Cell Anemia to Hearing Aids and Alopecia related to Chemotherapy.
After, a panel was held that brought together some thought leaders in the public health sphere, including:
- Dr. James Blessman, who spoke about the Citizenship Report card and the importance of eating more healthy foods, as in the Nutritarian Diet.
- Dr. Michele Cote, of the Karmanos Cancer institute who spoke about Lung Cancer screening
- Dr. Wassim Tarraf who discussed being a statistic himself, as an immigrant and adopting some of the unhealthy practices of living in America, like an unhealthy diet.
- Dr. Dawn Misra - of the Wayne State University Department of Family Medicine and Public Health who has an interest in perinatal health disparities.
- Julie Comstock-Gleason, who spoke about the importance of community health and community health workers as experts who know the community well. Currently, she's working on a project about heart health by building community health awareness groups and asking individuals to write themselves letters about what it means to be heart healthy.
- Dr. Phillip Levy is an emergency medicine physician at Henry Ford hospital and he discussed transformative moments in his career while taking care of patients in the emergency department at Lincoln Hospital. One of his quotes that stuck with me is when he referenced Roemer's law, or the idea that in an insured population, a hospital bed built is a filled bed. This means that whenever we as a community decide to build a hospital bed, it will not sit empty. This lead to further commentary about treating people who are ill rather than taking care of people so they remain healthy.
- Dr. Abdul El-Sayed, formerly of the City of Detroit Health Department, now making a run for Governor of Michigan had the audience repeat the definition of Public Health. Public Health is what we as a society do together to create healthy conditions. He also discussed how resources that keep people healthy are not evenly distributed. He noted that 40% of Detroiters don't have reliable access to transportation, creating an environment where people are not able to access basic services or meet their basic needs.
- Dr. Kim Jaffee of the School of Social work at Wayne State University discussed a pregnancy and nutrition surveillance system. Her team looks at the macro factors that affect pregnant women. She also is interested in low birthweight babies and the disparities in infant mortality rates between different communities. She is now examining the health disparities in the transgender community. One statement that she made that stuck with me is that Transgender patients who have to teach their doctor about who they are and what it means to be transgender are 3x's less likely to access care when they need it.
Health Equity is a big reason why we do what we do at Plum Health. We lower the barriers to excellent primary care services by making healthcare more affordable. We lower the costs of medications and lab testing by delivering these services at cost, saving our patients thousands of dollars each year. If more primary care doctors are able to practice in this Direct Primary Care model, we could truly make healthcare more affordable and accessible for all people.
Thanks for reading and have a wonderful day,
- Paul Thomas, MD