Plum Health Blog
Dr. Paul Thomas Speaks at the Dr. Morris S. Brent Lectureship
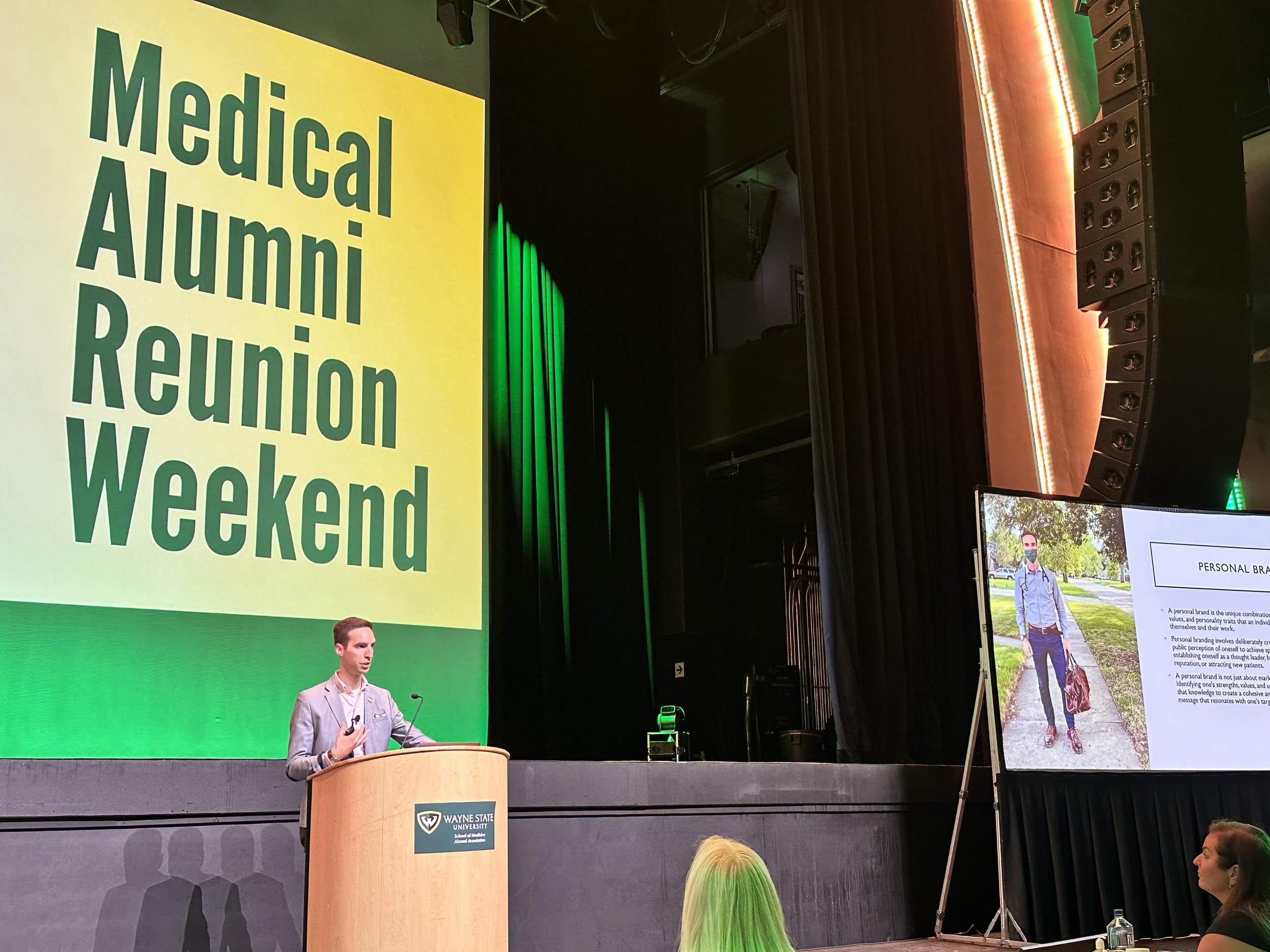
This month, Dr. Paul Thomas spoke at the Dr. Morris S. Brent Lectureship, a part of the Wayne State University School of Medicine’s Alumni Reunion Weekend activities. In the lecture, Dr. Paul Thomas discussed best practices for personal branding, and why it is important for doctors to become physician leaders, and build the platforms that can help them educate other doctors and the community about important issues in medicine.
This session will focus on developing a personal brand for physicians. What is a personal brand? How can you leverage your personal brand to attract new patients? How can you own your own brand and content? These topics and more will be addressed in this session!
Dr. Paul Thomas talks about Personal Branding at the WSU SOM Alumni Reunion Weekend during the Morris S. Brent Lectureship.
To watch the full lecture, head to the 2:14 (2 hour, 14 minute) mark in the YouTube video below:
Laceration Repair and Other Urgent Care Services at Plum Health DPC
Laceration Repair and Other Urgent Care Services at Plum Health DPC
At Plum Health DPC, we understand that accidents and injuries can happen at any time, and we are here to help our patients when they need it most. Our team is equipped to handle a wide range of urgent care needs, including laceration repair.
Lacerations, or cuts, can range in severity from small, shallow wounds to deep, jagged injuries that require surgical repair. No matter the severity of the laceration, it is important to seek medical attention as soon as possible to prevent infection and minimize scarring.
At Plum Health DPC, our team is skilled in laceration repair and can provide the necessary care to help our patients heal quickly and properly. Depending on the location and severity of the laceration, we may use sutures (stitches) or adhesive skin closures to close the wound. We will also clean the wound and provide any necessary antibiotics to prevent infection.
Furthermore, if you haven’t had a recent TDaP booster (a tetanus, diphtheria, and acellular pertussis vaccine), we will provide you with this necessary protection. If dirt or debris gets into the wound, tetanus can result. Getting the TDaP vaccine at the time of the laceration repair can prevent tetanus from occurring.
In addition to laceration repair, we also offer a range of other urgent care services at Plum Health DPC. These may include treatment for minor injuries, such as sprains and fractures, as well as management of acute illnesses, such as colds and flu.
If you or a loved one is in need of urgent care, don't hesitate to contact us at Plum Health DPC. Our team is here to provide the care you need, when you need it most.
Direct Primary Care Doctor in Detroit with Concierge Service
Direct Primary Care Doctor in Detroit with Concierge Service
Over the weekend, I made a house call to Ford Field.
Most of our house calls are to help regular Detroiters with the type of affordable and accessible health care services that we are known for at Plum Health.
If you don’t know about our direct primary care service, we offer excellent medical services at a monthly membership. We have an in-house pharmacy and we dispense medications, we offer a wide variety of procedures (biopsies, pap smears, toe nail removal, BOTOX), and we are able to draw labs and have the lab results back for our patients next day.
Most people use our Plum Health service because we can cut out the middle man and deliver a seamless primary care experience for an affordable price.
Every once in a while, we help a visiting executive, athlete, artist, or performer who needs our medical care and attention.
We have taken care of CEOs who require PCR testing with a rapid turnaround, we have taken care of artists who are visiting and who need help before an important gallery opening, and we’ve taken care of performers who need treatment before their big show here in Detroit.
These VIPs use our Plum Health service because we have the time in our schedule to accommodate their needs, we bring our medical care to them, and we give them a seamless experience without hassles. They might call it concierge medicine, but we prefer Direct Primary Care!
Happy Thanksgiving and thank you for considering Plum Health DPC for your health care needs!
-Dr. Paul Thomas with Plum Health DPC
Appreciation Post for Dr. George Costea
When I was 17 years old, I started volunteering at Cass Clinic, associated with the Cass United Methodist Church. This was about 2004, and it was a life changing experience. As a high school student, I got to work with and learn from medical students at Wayne State University School of Medicine as they took care of patients who were uninsured, underinsured, homeless, and elderly folks who couldn’t drive to another clinic.
After each patient encounter, we would give a presentation to Dr. Costea, who waited patiently for us to share the important clinical information, and who helped guide our management and care with an in-house pharmacy, dispensing blood pressure medications and diabetes medications alongside clinical pearls and clinical wisdom.
We were able to take care of about 30 to 50 patients each day, working in teams of 2 or 3 students, and seeing one patient at a time. We got to spend 30 minutes to an hour with each patient, and listen to their stories. They allowed us to learn from them with otoscopes, blood pressure cuffs, our stethoscopes, and an index card medical record system as many patients returned each week or each month.
From this experience, I knew that I wanted to become a doctor, not just any doctor, but a doctor like Dr. George Costea. Dr. Costea seemed to be infinitely knowledgable about every medication stocked in that backroom pharmacy, he was unendingly patient, and faced difficult situations in the clinic with unmatched equanimity.
When I eventually finished college and made it into Wayne State University School of Medicine, I continued to volunteer at the Cass Clinic, to serve the patients there and to learn from Dr. Costea. When it came time in my third year of medical school to rotate through a family medicine office, I had the privilege of rotating through Dr. Costea’s family medicine practice.
To say that my experiences working with and learning from Dr. Costea shaped me and shaped my career in medicine would be a gross understatement. His presence at the Cass Clinic is the single biggest reason that I had the opportunity to make it into medical school and to become a physician. Further, his model for care inspired me to start Plum Health.
Unfortunately, Dr. Costea passed away on September 19th, 2022.
Dr. Costea worked with hundreds or maybe even thousands of pre-medical students and medical students as they served patients in the Cass Corridor. He started the clinic in the early 1980’s as a part of the free health care movement, and volunteered just about every Saturday for more than 40 years. Dr. Costea’s example - his care, his selflessness, his humility, his patience, and his willingness to teach - will stay with me forever.
Thank you Dr. Costea!
-Paul Thomas, MD
Dr. George Costea at the Cass Clinic in Midtown Detroit.
From Wayne State University School of Medicine:
George Costea, D.O., founder of the Cass Clinic and attending physician for more than 40 years, died Sept. 19. Dr. Costea dedicated nearly every Saturday morning since the early 1980s to providing free health care to Detroit's poor and underserved. Dr. Costea taught hundreds of Wayne State University School of Medicine students during those years and demonstrated selflessness and commitment to serving the community. Cass Clinic is in need of physicians interested in volunteering their time. If you are interested in participating or need more information, please contact Rob Sherwin, M.D. at rsherwin@dmc.org.
Paul Thomas MD in the USA Today
Back in 2013, Dr. Paul Thomas helped start an organization called Street Medicine Detroit.
Street Medicine Detroit is a student-run organization that delivers primary care medical services to homeless and uninsured people on the streets of Detroit, in parks and in church basements, warming centers and homeless shelters. Street Medicine Detroit is a lifeline for folks who are living on the streets.
Medical Students from Wayne State University School of Medicine run the Street Medicine Detroit program and deliver medical care and compassion to people who are homeless, unsheltered, or without permanent housing.
When I was a fourth year medical student at Wayne State University School of Medicine in 2013, I helped a second year medical student named Johnny Wong start the organization. We went on "street runs" to deliver medical care to homeless people.
During one of those runs, a journalist named John Wisely followed our work and wrote about it in the USA Today.
I've been reflecting about the meaning of our work at Plum Health DPC and it has deep roots in the advocacy and volunteering that I engaged in before, during, and after medical school.
I turned the newspaper article from the USA Today into a plaque that I hang in my office as a reminder to keep meeting people where they are at, to keep delivering compassionate care, and to keep striving to make health care affordable and accessible for everyone.
Thanks for reading and have a wonderful day.
- Paul Thomas, MD with Plum Health DPC
Ganglion Cyst Drainage in Detroit
Ganglion Cyst Drainage at Plum Health DPC in Detroit
At Plum Health DPC in Detroit, we take care of a variety of health concerns. We are Family Medicine Specialists and we help our patients with a variety of health problems.
At Plum Health, we perform many procedures. One of those is a Ganglion Cyst Removal. This procedure takes a few minutes but it can be a tremendous relief.
A ganglion cyst is a pocket of fluid that builds up adjacent to a tendon. The Fluid inside the cyst is viscous and clear. The ganglion cysts are usually not painful, but they can be irritating if you wear a watch. They can also cause people to be self conscious or to wear long sleeves to cover them up.
At our clinic, we clean off the skin overlying the ganglion cyst and we use an 18 gauge needle to draw out the cystic fluid. This helps to relieve the symptoms for the patient.
After this procedure, there is a 50% chance that the ganglion cyst will resolve. For the other 50% of patients, the ganglion cyst will refill. Usually the ganglion cyst will refill slowly over time.
Plum Health Featured on Fox 2 News Detroit for Lowering the Cost of Insulin
Plum Health Featured on Fox 2 News Detroit for Lowering the Cost of Insulin
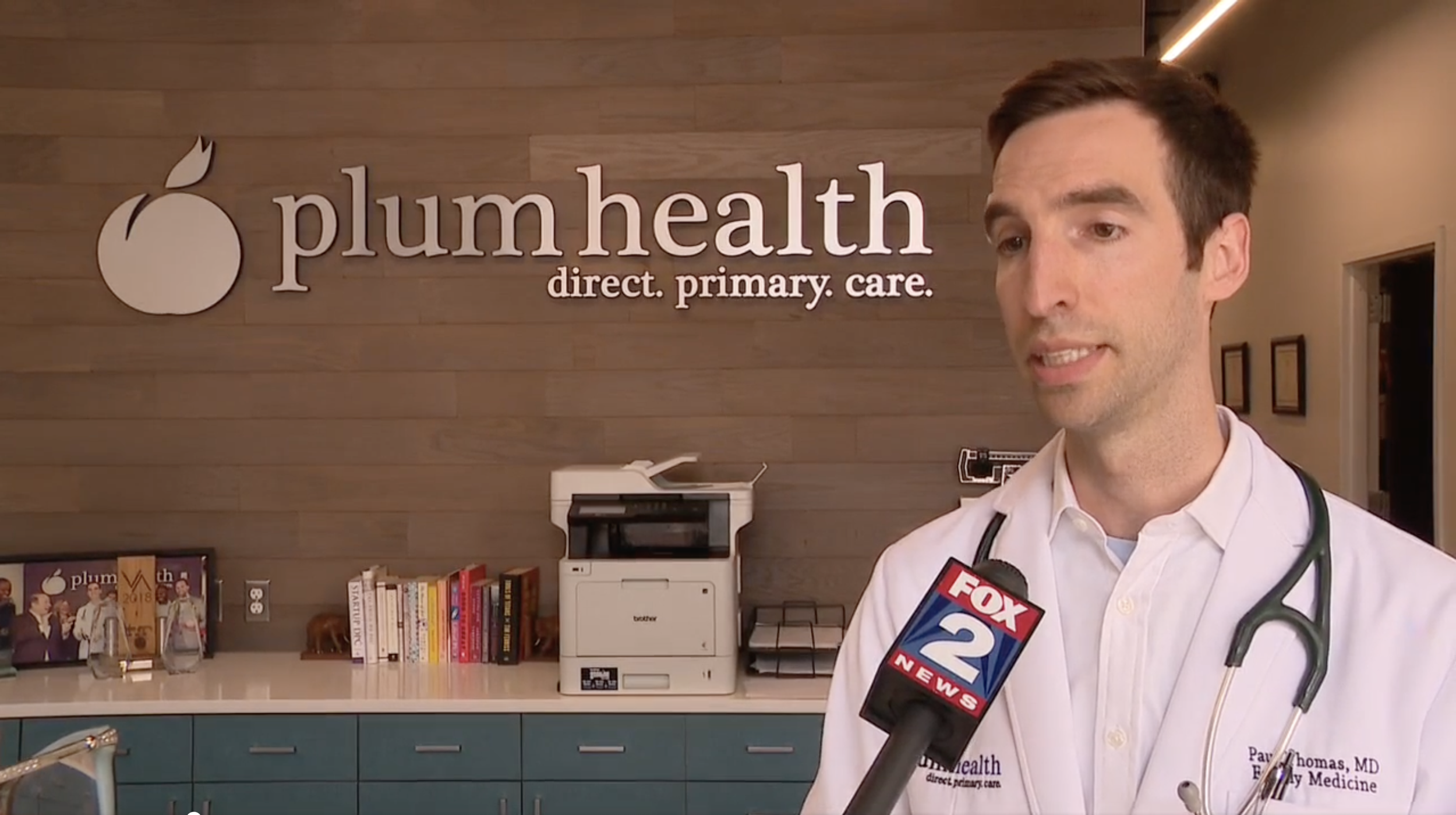
Yesterday, Plum Health DPC was featured on Fox 2 News Detroit for lowering the cost of insulin in Detroit and beyond.
MANAGING DIABETES IN DETROIT
Diabetes care can be difficult and expensive, especially if you’re uninsured. If you’re uninsured and trying to access diabetes care, patients can face the following costs:
$150 for a primary care visit
$150 to check hemoglobin a1c
$150 to check blood sugar via a comprehensive metabolic panel
$300 for insulin at the pharmacy
$10 for Metformin (Glucophage) at the pharmacy
At our Plum Health office, we dramatically lower the cost of these vital services to help our diabetic patients manage their blood sugar.
$55 to $75 monthly for as many primary care visits as it takes to manage your diabetes
$6 to check hemoglobin a1c
$6 to check blood sugar via a comprehensive metabolic panel
$0 for insulin at our Plum Health clinic as we get several free samples from industry
$0.30 to $0.60 for Metformin (Glucophage) at our Plum Health clinic
What makes this pricing difference even more important is that folks with diabetes need to check their hemoglobin a1c every 3 to 6 months to ensure that they are managing their diabetes effectively.
Dr. Paul Thomas of Plum Health DPC being interviewed by Fox 2 News about the high cost of insulin in Detroit and beyond. People routinely pay $125 for 1 pen of long-acting insulin like Tresiba. At our Plum Health DPC office, we are able to get free samples so that the cost is $0 for our members at Plum Health. Our mission is to make health care affordable and accessible, and lowering the cost of insulin is just one way that we achieve that mission.
Here’s our social media post about Insulin Costs in Detroit:
These insulin pens are $125 a piece at your local pharmacy. 🤑 💰
They should be capped at $35 a piece, but that protection was removed by Congress this week. 🤯😭🤢🤮
Fortunately, we get free samples from industry to help our patients at Plum Health DPC ✅
Tune in to Fox 2 News at 6 pm with Veronica Meadows as we talk about what’s broken in our healthcare system and what we’re doing to fix it 💯
#PlumHealth #DirectPrimaryCare #FamilyMedicine #insulin #drugprices #healthcare
Here’s what Fox 2 News Detroit wrote on their webpage about the story:
FOX 2 - For those who have diabetes, many know the struggle of paying for insulin.
"This can be $125 per pen at the pharmacy," said Dr. Paul Thomas. "In the United States there’s seven million people who need to take insulin and 25 percent of those cannot afford the insulin, they need to manage their diabetes."
For Raphael Wright, that stress hits close to home. A Detroit entrepreneur — Wright says at first he didn't have health insurance. He says his out-of-pocket cost for insulin used to be around $300 a month.
"It was a punch in the gut, I did not feel good," he said. "I am on the fringe because now I'm worried about getting my lights cut out. You need electricity to keep insulin cold."
Senator Debbie Stabenow (D) says starting in January the inflation reduction act will help more than three million in the US afford insulin.
"If you receive your health care through Medicare your insulin medicine will be capped your cost at $35 a month," she said.
But Senate Republicans stripped a provision that would have capped the price of insulin in the private marketplace. That cap also doesn't apply to people who don't have insurance.
"I think we should have a $35 cap for all Americans because there are a lot of people who are uninsured - they make too much money to qualify for Medicaid and not enough money to buy private insurance," said Dr. Thomas. "And even if you have private insurance your deductible could be $7,000."
Thomas is the founder of Plum Health Direct Primary Care in Corktown. He says thanks to free samples, his patients don't pay for insulin.
Thomas says his mission is to make healthcare accessible to everyone — especially diabetes patients. He says the results are devastating for those who are priced out of insulin.
"They’re going without, because of that high cost, and essentially this leads to really bad outcomes: Diabetic retinopathy which can cause blindness, diabetes does damage to your blood vessels, which can lead to early heart attacks and strokes," he said.
Thomas says diabetes is the number one cause of amputations and blindness in the United States. He says that is one more reason why insulin needs to be affordable for everyone.
Reproductive Health Care in Detroit Part Two
Reproductive Health Care in Detroit
In an ongoing conversation about reproductive health care, I will be giving some facts and figures about abortion in this blog post. Abortion is a flashpoint in our society; as always, I will be taking a measured, evidenced-based approach to this issue as I am a family medicine physician, and I rely on evidence to make clinical decisions.
The conversation here is adult/mature; the content here may be triggering for some readers. The descriptions of abortion here are not typically discussed in polite society. If you have concerns, read no further.
This week, I discussed much of the following information in the Daily Detroit podcast with Jer Staes. If you’d rather listen to this information, you can do so here:
You can listen to the podcast episode, here.
Abortion Rate in the United States
In 2020, the Census Bureau estimated that women made up about 50.7 percent of the population — some 167 million people. In the United States in 2020, the population of women ages 15-44 was 64,543,832.
In 2019, 629,898 legal induced abortions were reported to CDC from 49 reporting areas.
The majority of abortions in 2019 took place early in gestation:
92.7% of abortions were performed at ≤13 weeks’ gestation;
6.2% of abortions were performed at 14–20 weeks’ gestation
fewer than 1.0% of abortions were performed at ≥21 weeks’ gestation.
Early medical abortion is defined as the administration of medications(s) to induce an abortion at ≤9 completed weeks’ gestation, consistent with the current Food and Drug Administration labeling for mifepristone (implemented in 2016).
In 2019, 42.3% of all abortions were early medical abortions.
I think that knowing how many abortions take place per year is important. In short, there are 629,898 abortions for 64,543,832 women of childbearing age (15 to 44 years of age). That means that less than 1% of American women have an abortion each year (629,898 abortions / 64,543,832 women = 0.975% of women have an abortion every year.
And it’s important to know when these abortions take place during pregnancy. 92.7% of abortions take place at 13 weeks or less, or when the baby is the size of a lemon.
When is a Fetus Viable Outside of the Womb?
Doctors now consider 22 weeks the earliest gestational age when a baby is "viable," or able to survive outside the womb. But this is still extremely premature, and a baby born at this age will need a great deal of medical attention. Even if s/he survives, the risk of permanent disability is very high.
What are Common Scenarios When Abortion May Be Needed to Preserve the Health of the Mother or the Developing Fetus?
Ectopic pregnancy
Many people have heard of an ectopic pregnancy. An ectopic pregnancy is a pregnancy in which the fetus develops outside the uterus, typically in a fallopian tube. An ectopic pregnancy always ends in pregnancy loss. About 1 to 2% of all pregnancies in the United States are ectopic pregnancies.
The image on the left shows an embryo that is implanted correctly within the uterus. The right hand image demonstrates the various locations of an ectopic pregnancy. An ectopic pregnancy in the fallopian tube is called a tubal pregnancy, and can result in severe pain and damage to the fallopian tube.
Attribution: By BruceBlaus - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=44897672
An early ectopic pregnancy without unstable bleeding is most often treated with a medication called methotrexate, which stops cell growth and dissolves existing cells. The medication is given by injection.
Salpingostomy and salpingectomy are two laparoscopic surgeries used to treat some ectopic pregnancies. In these procedure, a small incision is made in the abdomen, near or in the navel. Next, your doctor uses a thin tube equipped with a camera lens and light (laparoscope) to view the tubal area.
In a salpingostomy, the ectopic pregnancy is removed and the tube left to heal on its own. In a salpingectomy, the ectopic pregnancy and the tube are both removed.
Which procedure you have depends on the amount of bleeding and damage and whether the tube has ruptured. Also a factor is whether your other fallopian tube is normal or shows signs of prior damage.
In the context of an abortion ban, doctors may hesitate to intervene on behalf of a woman with an ectopic pregnancy. The doctor may have to contact the legal department at the hospital to ensure that they are not running afoul of the new rules and regulations. This hesitation and the time it takes to clear the legal department will likely result in more ruptured ectopic pregnancies, which will lead to damage to women’s reproductive organs, a decreased chance of healthy pregnancy in the future for these affected women, and potentially death for the mother in cases of sepsis or infected internal organs.
This is a real world consequence of this abortion ban, and this has already happened. Here’s a story from a nurse/health care worker on Instagram who relates how an ectopic pregnancy was not treated in a timely manner, and resulted in a rupture and then 600 mL of blood in the abdomen of the expectant mother, which came close to causing death for the mother.
A story posted on Instagram about a ruptured ectopic pregnancy and the real consequences for an expectant mother.
Here’s a similar story from Kaiser Health News about the importance of prompt care for ectopic pregnancy.
Incomplete Miscarriage
Miscarriage occurs in 8–15% of clinically recognized pregnancies and in ~30% of all pregnancies. Increasing maternal age is associated with an increasing risk of miscarriage. Many women may have a miscarriage and not even know it - they may experience a miscarriage as a heavy period a few weeks after their normal period. Other women may have a pregnancy, have a positive pregnancy test, and then miscarry a few weeks later.
These early miscarriages are often sad and painful, but don’t often require medical intervention as the mother’s lining of the uterus can slough off and expel the embryo/fetus/early pregnancy without retaining any tissue.
However, some pregnancies will experience a spontaneous abortion at 16 weeks or 18 weeks or 20 weeks, and the fetus/baby will be much larger. For whatever reason (usually a severe genetic problem) the baby will die in utero. This is not uncommon. The problem here is that some parts of conception (or body parts of the baby/fetus) can be retained, or some body parts can stay inside the uterus. If these products of conception are not removed, the uterus can be come infected and the mother could become septic and potentially die.
An incomplete abortion is the partial loss of the products of conception within the first 20 weeks. Incomplete abortion usually presents with moderate to severe vaginal bleeding, which may be associated with lower abdominal and/or pelvic pain. It is important to diagnose this early to make sure the patient expels all products of conception.
The overall incidence of spontaneous abortion is 10% to 15%. It is divided into early, <12 weeks, and late, >13 weeks.The causes of abortion are usually unknown but most commonly are attributed to fetal chromosomal abnormalities and the rest due to modifiable etiologies and risk factors. Treatment of incomplete abortion includes expectant, medical, and/or surgical treatment.Complications are rare but can be serious such as sepsis from the retained product, hemorrhagic shock, and uterine rupture. The prognosis for these patients is generally good with a proper workup, close obstetric follow-up, and patient education. [Source]
In patients with conception fragments at the cervical os, a clinician can remove the fragments with forceps to help initiate the process of hemostasis, facilitate uterine contractions, and decrease vagal stimulation. This will prevent cervical shock. In plain English, sometimes body parts of the fetus/baby get stuck in the mom’s uterus/cervix and they need to be removed by the OB/GYN with forceps. This is a heart-wrenching scenario, but again, doctors need to act fast to remove these retained products of conception, otherwise the mom can get a severe infection and die.
Patients with an incomplete abortion and retained products of conception commonly have one or more of the following signs: uterine bleeding, pelvic pain, fever and uterine tenderness. Patients with hemorrhagic shock have obvious blood loss and those with septic abortion have signs of sepsis.
Here’s a story that was circulating on social media over the weekend. A patient had a 16 week gestation fetus/baby in her uterus. Her water broke early, and the baby started to come out of the woman’s uterus, then cervix, then vagina, resulting with the fetus/baby’s foot resting outside of the vagina. In a case like this, the baby will die - it cannot be replaced into the uterus. However, this doctor is practicing in a state that has banned abortion. Because the baby’s heart is still beating, they have to wait until the baby dies before the retained products of conception/fetus/baby can be removed. This is harrowing.
In some cases, an early pregnancy at 8 or 10 or 12 weeks of gestation can die in the womb, but remain in the womb without clearing in a timely manner. This can lead to physical and emotional pain for the mom, and has a risk for infection/sepsis and death in the mother as well. In these cases, doctors can go in and remove the embryo/fetus with a vacuum suction or a dilation and curettage procedure, where the baby is scraped out of the uterus by the doctor.
To make this real, here’s a heartfelt story from NFL player Nick Sundberg about their family’s experience with needing an abortion (dilation and curettage) after his wife miscarried on two separate occasions.
In Vitro Fertilization (IVF)
Depending on the language and interpretation, a state law could curtail access to fertility treatments, and in some cases, make the practice of freezing or discarding unused embryos in In Vitro Fertilization illegal.
The language could affect fertility procedures in two ways.
The first impact could be on selective reduction, or multifetal reduction, the practice of reducing the number of fetuses in one pregnancy.
This procedure is not as common today but may occur if a woman undergoes hormone therapy, which could increase the number of eggs and result in triplets or quadruplets. In these cases, there is a chance the woman or embryos could be at greater risk of an unsuccessful pregnancy, which is why a fertility clinic may decide to reduce one or more of these fetuses. This could meet the definition of abortion in some states.
The more common practice, IVF, which results in half a million deliveries annually, is when eggs are extracted, fertilized and the embryos are formed in a petri dish outside of the body. The embryos are then genetically tested, and only the healthy ones are implanted, reducing the chances of selective reduction because they don’t have to implant as many at once. The unused embryos are either frozen and stored for later use, discarded during or after the process or donated for scientific research.
In some strict interpretations of the abortion ban, freezing or discarding embryos or donating embryos for scientific research could be criminalized.
Babies Without Developed Organs
Anencephaly is a severe congenital condition in which a large part of the skull is absent along with the cerebral hemispheres of the brain. Some women become pregnant and the baby develops without a brain.
Anencephaly is a rare type of neural tube defect that affects about 1 in 4,600 babies. There is no way to treat anencephaly. Babies born with this condition will die before or shortly after birth.
Spina bifida is a congenital defect of the spine in which part of the spinal cord and its meninges are exposed through a gap in the backbone. It often causes paralysis of the lower limbs, and sometimes mental handicap.
Cancer
Chemotherapeutic agents and radiation for cancer treatment can cause birth defects. Studies show there is a risk of birth defects when a woman becomes pregnant while getting or after receiving some types of chemotherapy, radiation therapy, and hormone therapy. In some cases, the risk can last for a long time, making getting pregnant a concern even years after treatment ends.
Rape or incest
Just 1% of women obtain an abortion because they became pregnant through rape, and less than 0.5% do so because of incest.
Does Banning Abortion reduce Abortion Rates?
According to data from the World Health Organization (WHO), the legality of abortion across the world actually has little to no effect on abortion rates throughout the world.
Legal or not, abortions can, will, and do take place.
The legality of abortion, however, does affect how safe those abortions are. Women who do not have access to a legal abortion frequently turn to illegal or "homemade" abortion options, which are typically much riskier, more dangerous, and less effective than legal options conducted by professional doctors in a clinical setting would be. (source)
Is abortion legal in Michigan right now?
Yes. Abortion is still legal in Michigan as long as the injunction is in place.
This is the latest email that I received from LARA or the Licensing and Regulatory Affairs of the State of Michigan:
On Friday, the U.S. Supreme Court overturned a woman’s constitutional right to abortion services. Under this decision, laws and court rulings in each state guide how health professionals provide abortions and abortion-related services. In Michigan, there is an injunction in place, based on a court order prior to Friday’s U.S. Supreme Court decision, that protects women seeking abortion services and the health care professionals assisting them. That order states, “Defendant [the Attorney General] and anyone acting under defendant’s control and supervision, see MCL 14.30, are hereby enjoined during the pendency of this action from enforcing MCL 750.14.” The order also provided that the Attorney General give immediate notice of the preliminary injunction to all state and local officials acting under her supervision. It is LARA’s position that abortion remains legal in Michigan because of the current injunction that prohibits enforcement of the 1931 law.
We understand that you may have some concerns about how continuing to provide medical and surgical services to women seeking abortion may impact your professional license. The Department of Licensing and Regulatory Affairs will not take any action against any health professionals for providing legal abortion services while the current injunction remains in place.
Thank you for your commitment to providing services to women in need and to all Michigan citizens. We will continue to update you as new information becomes available.
Bureau of Professional Licensing, Michigan Department of Licensing and Regulatory Affairs
Where can I Receive an abortion in Michigan right now?
To be clear, we do not perform abortions at our clinic. We do provide counseling, contraceptive care, pap smears, mammograms, women’s health care, and referrals for abortion when needed.
You can likely seek care from your OB/GYN at most major hospital systems or you can seek care from Planned Parenthood. If you are struggling to find options, please reach out to our office so that we can guide you through this difficult process.
How can we reduce abortion rates in michigan?
Abortion should be a last resort for women and for families. It is a difficult decision that can have long-lasting familial, physiological, and emotional effects. There are ways to reduce abortion rates if we want to and that looks like:
Access to free contraceptives
comprehensive sex education
universal health care
paid family leave
welfare funding
secure housing for all
closing the wage gap
funding education
According to the Colorado Department of Public Health and Environment:
The Colorado Family Planning Initiative drove a 50 percent reduction in teen births and abortions, avoided nearly $70 million in public assistance costs and empowered thousands of young women to make their own choices on when or whether to start a family.
A private donor’s investment in the state health department’s family planning program allowed us to train health care providers, support family planning clinics and remove the financial barriers to women choosing the safest, most effective form of contraception.
This initiative empowered thousands of Colorado women to choose when and whether to start a family.
Thanks in large part to the Colorado Family Planning Initiative:
Teen birth rate was nearly cut in half.
Teen abortion rate was nearly cut in half.
Births to women without a high school education fell 38 percent.
Second and higher order births to teens were cut by 57 percent.
Birth rate among young women ages 20-24 was cut by 20 percent.
Average age of first birth increased by 1.2 years among all women.
Rapid repeat births declined by 12 percent among all women.
Costs avoided: $66.1-$69.6 million.
In short, the above example from Colorado is an effective public health policy for reducing abortion. Banning abortion at a Federal level with little thought or care given to the nuances of pregnancy, ectopic pregnancy, miscarriages, etc… is an ineffective way to reduce abortion that will result in harm to the women of our country, their families, and our communities.
Thanks for reading,
-Dr. Paul Thomas with Plum Health DPC in Detroit, Michigan
Plum Health DPC Featured in Upcoming Alive in Detroit Documentary
Plum Health DPC Featured in Upcoming Alive in Detroit Documentary
Alive in Detroit is a documentary put together by my friend Shiraz Ahmed. He has been acutely interested in health access in Detroit and beyond and our mission of making health care affordable and accessible in Detroit resonated with Shiraz. Shiraz included our work in a forthcoming documentary about health care in Detroit called Alive in Detroit. He’s raising money for the film right now on his Kickstarter campaign, so please contribute if you have the time and the means as this will be a timely and insightful documentary.
Shiraz was recently interviewed on WDET here in Detroit to explain more about the project. Here’s what WDET said:
“Alive in Detroit,” directed by filmmaker Shiraz Ahmed, is an upcoming feature-length documentary about the fight against chronic diseases such as cancer, heart disease and diabetes in the city. This story is a celebration of Detroiters and the work they do to heal their communities of illnesses while also providing them with protection and rights.
The film features a patient, a pastor and a physician whose stories inspire hope but also mask deeper inequities in the health care safety net. It’s a product of the city’s creative ecosystem, benefitting from programming by the Detroit Design Festival, the Freep Film Festival and Documenting Detroit.
“The pandemic’s really exposed all these cracks we have in our system,” he says. “I started this film before the pandemic, and then the pandemic just crystalized the themes I was looking at. It really gave me motivation – especially at a really depressing time when there was not a lot else to do to keep moving forward – because if we don’t address these inequities, another pandemic will happen and more people will keep dying.”
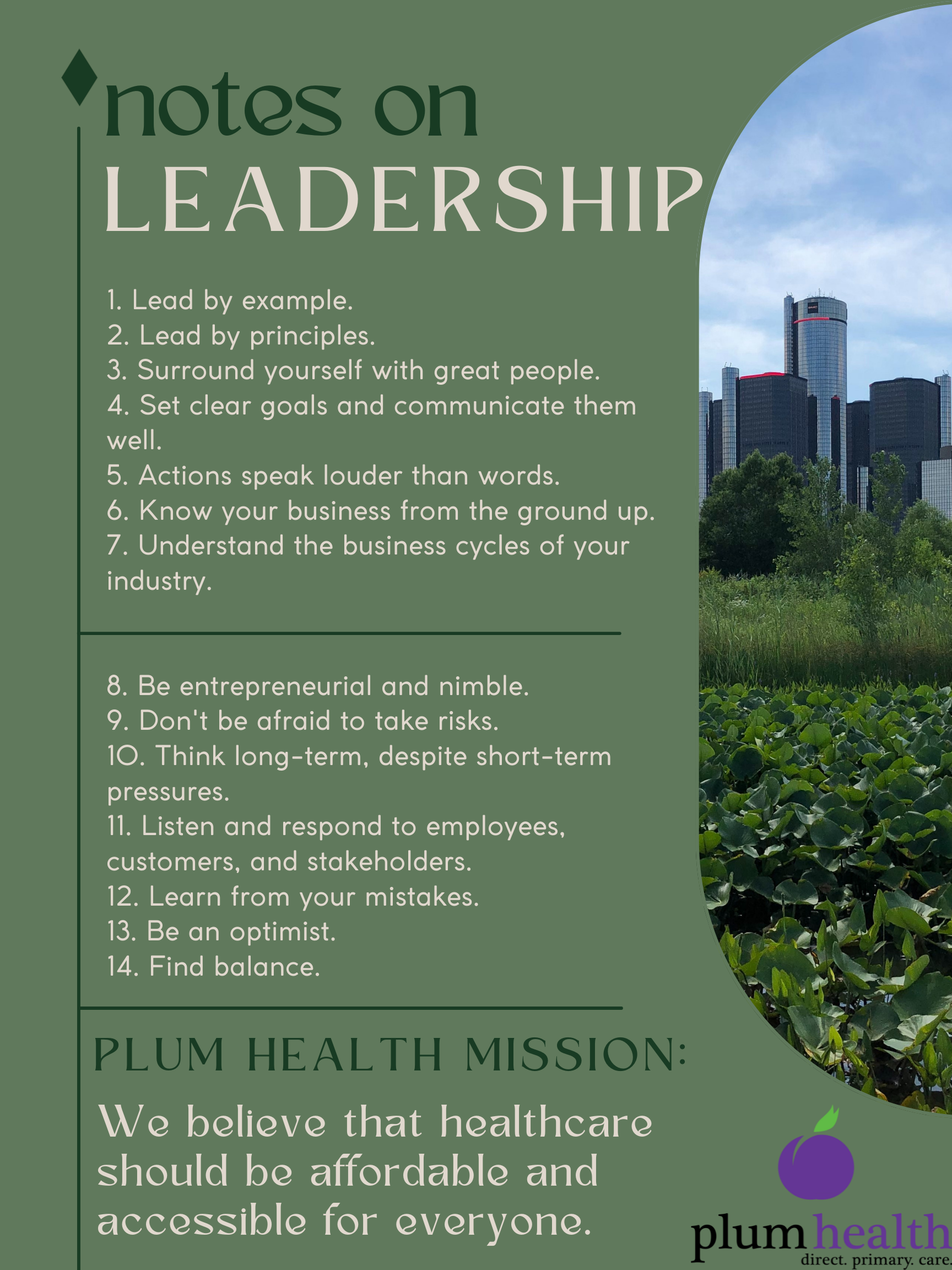
Leadership at Plum Health DPC
I have this grainy copy of a photo of a document above my desk that serves as a reminder about leadership and how I operate my business at Plum Health DPC. I look at it every day, and it helps me focus on how I conduct myself to create a successful organization. I thought I’d share it with you today!
Notes on Leadership, a reminder to myself:
1. Lead by example.
2. Lead by principles.
3. Surround yourself with great people.
4. Set clear goals and communicate them well.
5. Actions speak louder than words.
6. Know your business from the ground up.
7. Understand the business cycles of your industry.
8. Be entrepreneurial and nimble.
9. Don't be afraid to take risks.
10. Think long-term, despite short-term pressures.
11. Listen and respond to employees, customers, and stakeholders.
12. Learn from your mistakes.
13. Be an optimist.
14. Find balance.
Notes on Leadership at Plum Health DPC
Detroit Demo Day - Plum Health DPC Two Years Later
Back in 2021, we won Detroit Demo Day - we competed with several other businesses and we won $50,000 to help us get to the next level.
Since then, we've:
Tripled the number of patients served
Built out a brand new office in Detroit's Corktown Neighborhood
Opened up a second office in Farmington Hills
Created a more sustainable business
If you want to accelerate the growth of your business, apply for Demo Day pitch competition as it can be rocket fuel for your next big move! More details, here.
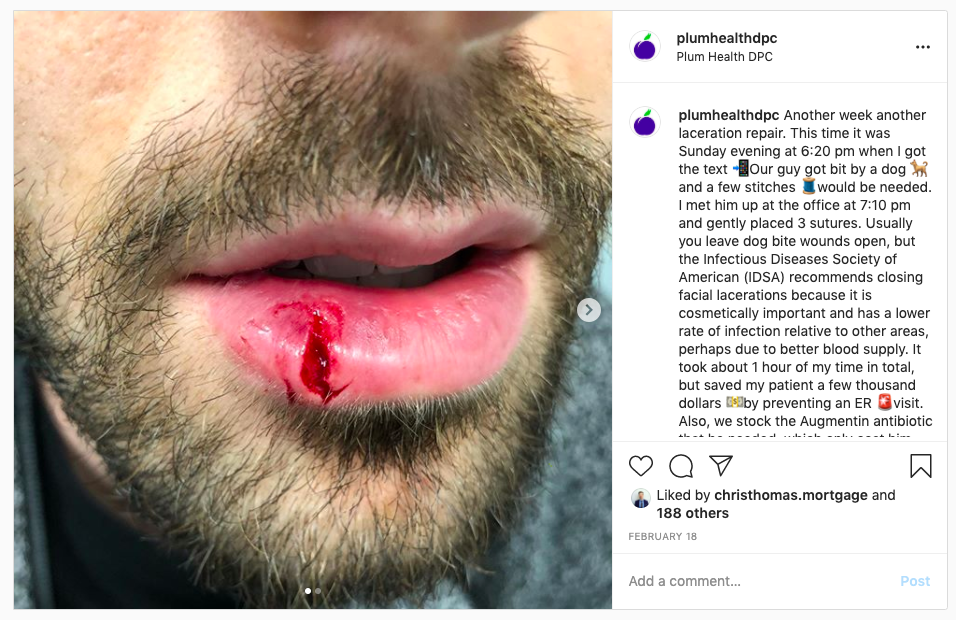
Warning: Dog Bites Can Be Painful and Costly
Dog bites can be painful and costly, but it doesn’t have to be that way. We go above and beyond for our patients to try to prevent any unnecessary emergency department visits. We can treat dog bites, cuts, asthma attacks, and several other urgent care-type concerns in our office. This goes a long way for our patients, giving them the assurance that their doctor is available to them and protects their pocket books from over charges at the hospital.
Thanks for reading and have a wonderful day - Dr. Paul Thomas with Plum Health DPC
Dog Bite Laceration on lower lip before
Dog Bite Laceration on lower lip, after 3 sutures at Plum Health DPC in Detroit Michigan
Detroit Family Medicine Office Open During the Coronavirus Pandemic
Detroit Family Medicine Office Open During the Coronavirus Pandemic
We’ve received a lot of questions about whether or not we’re open during this Coronavirus Pandemic. Yes, we are open during the pandemic and we plan on remaining open for as long as it’s safe to treat patients. We are taking several precautions to keep our patients safe during this time.
We are open and we are continuing to offer telemedicine appointments for all of our existing patients and new members. We are also offering in-person appointments to our patients when necessary. For example, we recently sutured a dog bite for one of our patients to prevent an emergency room visit.
Where we can, we will treat patients in the office to save them money and decrease their risk of Coronavirus at hospital and urgent care settings. We are also open for medication pick ups and lab draws for patients who need medication refills or their necessary lab work completed, like hemoglobin a1c testing for our diabetic patients. We are coordinating testing for COVID-19 and we will soon have antibody testing in our office.
How Has COVID-19 Changed Our Business?
We have always been able to text and email our patients, and conduct some visits by phone and video chat. We never thought that we'd have to completely rely on digital communication to take care of our patients, but COVID-19 changed all of that.
We’re used to seeing patients in our office face-to-face and developing genuine relationships with the people we take care of during that process, but due to COVID-19 we've been limiting our face-to-face visits as much as possible to limit the potential spread of the Coronavirus. The health and safety of our patients is paramount and by limiting our contact with patients in the office, we're doing our part to limit the spread of the virus.
Thanks for reading and have a wonderful day,
-Dr. Paul Thomas with Plum Health DPC
Dr. Raquel Orlich Reaches A Major Milestone
This week, Dr. Raquel Orlich reached a major milestone - she now has 200 patients in her practice panel. Here’s what we said on Facebook:
A huge congratulations 🎈 to Dr. Raquel Orlich. She joined our Plum Health direct primary care practice on July 1st 2019 and she’s already reached 200 patients in her panel!
Dr. Raquel 👩🏻⚕️ is intelligent, compassionate, and a relentless advocate for the health and wellbeing of her patients. She focuses on chronic musculoskeletal issues, women's health, and preventive medicine.
We’re lucky to work with you, and our patients are fortunate to have such a kind and caring doctor looking out for their best interests. 💯
Of note, Dr. Raquel has room for about 500 patients in her practice panel, so if you’d like to sign up to be one of her patients, head over to our Schedule Now page to get started!
-Drs. Paul Thomas and Raquel Orlich with Plum Health DPC
Dr. Paul Thomas at the Future of Family Medicine Conference
Last month, I had the opportunity to speak with over 100 students and residents interested in the specialty of Family Medicine. This was at the aptly named “Michigan Future of Family medicine Conference” hosted by the Michigan Academy of Family Physicians. The event was held at Michigan State University and hundreds of students were able to attend on a Saturday morning in October.
The invitation for the fifth annual Michigan Future of Family Medicine Conference, hosted by Michigan State University and the Michigan Academy of Family Physicians (MAFP).
For students, it can be hard to get excited about the future of Family Medicine. Family Physicians work long hours, have to deal with tons of insurance bureaucracy and red tape, and earn less than their colleagues in other specialties. It can leave students deflated.
Dr. Paul Thomas of Plum Health DPC speaks at the Michigan Future of Family Medicine Conference 2018 Panel on Career Options, taken from the Michigan Academy of Family Physicians’ (MAFP) twitter account, here: https://twitter.com/MIFamilyDocs/status/1051106817705725953
However, I find that when I speak about Direct Primary Care and the opportunities that a DPC model of care can provide, students are energized and excited about the future of family medicine. You see, Family Medicine Doctors have the most tools in their tool set and can have the biggest impact on the community level - we lower admission rates to hospitals and decrease the cost of care for our patients. We also lower the rates of disease and death rates from disease.
But, as mentioned previously, Family Medicine is less desirable from the student’s perspective as it pays less and is a difficult job because of insurance hassles.
I think our profession, Family Medicine, is at a real moment of crisis, but also at a crossroads for opportunity. We can continue to be a part of the healthcare industrial complex, billing and coding, racking up charges on our patients, or we can adopt the Direct Primary Care model and serve our patients and our community with affordable and accessible health care services that are more just and compassionate in their delivery.
That’s my message, I’m glad to have had the opportunity to share it, and I’m very happy to have seen it resonate with so many energetic and eager medical students and residents.
Thanks for reading, and have a wonderful day,
-Dr. Paul Thomas, MD with Plum Health DPC, a Direct Primary Care service in Southwest Detroit
Dr. Paul Thomas of Plum Health DPC speaks at the Michigan Future of Family Medicine Conference 2018 Panel on Career Options, taken from the Michigan Academy of Family Physicians’ (MAFP) twitter account, here: https://twitter.com/MIFamilyDocs/status/1051097050086035456
I had the pleasure of speaking to an audience of over 100 + Medical Students and Medical Residents at the Michigan Future of Family Medicine Conference in October 2018. I shared the stage with Dr. Sheala Jafry, Dr. Fatin Sahhar, and Dr. Amy Keenum. The event was held at Michigan State University and hosted by the Michigan Academy of Family Physicians (MAFP).
How is Plum Health Making an Impact?
Family Medicine Doctor Reaching Out in Detroit
Dr. Paul Thomas speaking to elementary school students at Munger Elementary/Middle School on Detroit's West Side during Career Day.
This week, I engaged in two outreach events, one at Munger Middle Elementary/Middle School on Detroit's West Side and one at the Northwest Activities Center in NW Detroit. The first event had me speaking to a group of about 30 elementary school students, sitting cross-legged on a gym floor. We talked about what it takes to become a doctor, the dreams that they had for their futures, and the steps that it would take to achieve those dreams. They even made me a nice gift for coming out - a small paper doctor.
Dr. Paul Thomas at Munger Elementary/Middle School on the West Side of Detroit.
The event at the Northwest Activities center had me speaking to about 100 senior citizens who had innumerable questions about health and wellness. They asked me about everything from high blood pressure, to diabetes, to nutrition, exercise, arthritis, and declining cognitive function. Also at this event, the community had organized fresh food distribution.
Dr. Paul Thomas at the Northwest Activities Center in NW Detroit after speaking to a group of senior citizens about health and wellness.
Both were inspiring in different ways, and also showed how we can make a big impact by reaching out to the community and educating people from elementary age to senior citizens. I think a lot about impact, and how we're making a positive impact in the community, and I wanted to share an essay I wrote earlier this month:
How a Family Doctor Makes an Impact
The problem that I am solving is access to affordable medical care, not just for individuals, but also for small businesses and communities. On the individual level, I cannot count the number of people who have presented to our clinic to establish care with a family doc for the first time in years, sometimes even decades. They feel comfortable because the price point is understandable, services and charges are transparent, and we've created a welcoming environment for all people.
I’ll give the example of the lifelong Detroit resident who had a uncontrolled blood pressure, who avoided medical care because the cost was simply too high. She signed up for a membership with us, and we are managing her blood pressure with medication that costs under $2/month. She is now at goal, and cried in our office after reaching this critical threshold.
Next, we’re solving a big problem for small businesses. Small business owners want to provide services and benefits that will help them attract and retain employees, and often times traditional health insurance products are financially out of reach. Rather, they choose to provide Plum Health and our health care services for their employees: an affordable product that’s understandable and easy to access for their workers. We are now seeing small businesses that are proud to offer our service as a benefit to their employees as a mean of attracting and retaining talent.
Finally, we’re solving the problem of neighborhood-based primary care services in Detroit, a city that is critically underserved from a primary care perspective. There are fewer than 100 primary care doctors in the City of Detroit, equating to roughly 1 doctor for every 6,300 residents. We are meeting a significant need in our Southwest Detroit location by serving a community that otherwise would not have access.
Thanks for reading, and have a wonderful day,
- Dr. Paul Thomas with Plum Health DPC in Detroit, Michigan
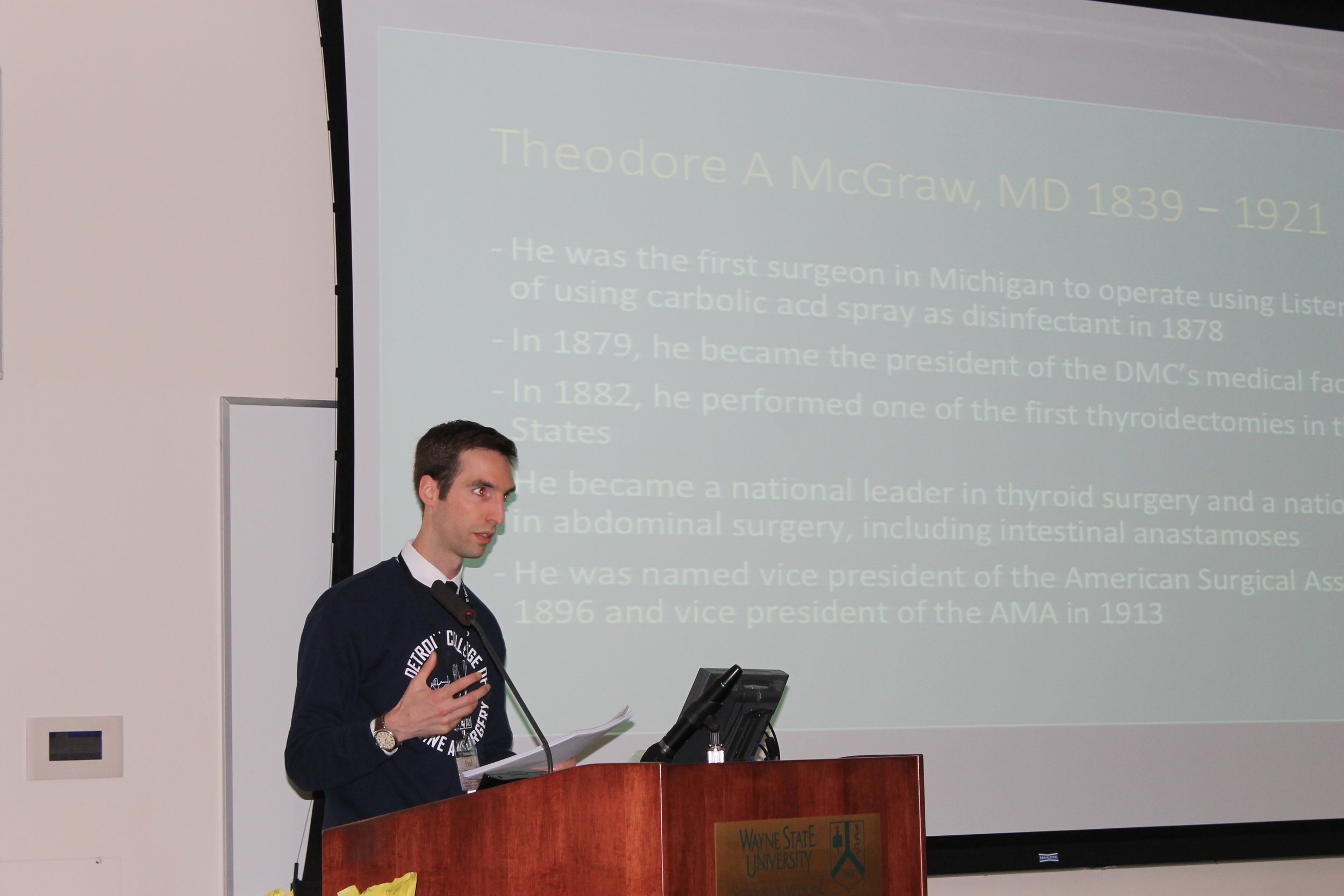
The History of Wayne State University School of Medicine
This week, I was invited to give a presentation on the history of Wayne State University School of Medicine during its Sesquicentennial Celebration. Yes! The WSU SOM is 150 years old, and it has a rich history of diversity, inclusion, and innovation that should be celebrated. Interestingly, the history of the Medical School is the history of the University, as the University grew out of the Medical School. While I can't cover the entire history in a single blog post, I will give some highlights from the early years of the college below. When the full presentation is released later this year, I will post it to the blog as well.
Theodore A. McGraw, MD, founder of the Detroit Medical College, which would later become Wayne State University School of Medicine.
The Detroit Medical College was founded in 1868 by five returning Civil War Veterans. One can only imagine the horrors that they saw on the battlefield and you can also imagine the inadequacy that they felt in treating wounded soldiers. In the 1860's, aseptic surgical techniques were only beginning to be used and anesthesia was not fully understood.
Can you imagine what it might have felt like to be a battlefield clinician, and not having the proper tools or training? Dr. Theodore McGraw, founder of the Detroit Medical College is quoted as saying: "I had discovered in my two years of army activity that I was deficient in that exact knowledge of anatomy that was essential to good surgery. The advent of antiseptic and aseptic surgery, besides, had opened a new field for operative work, that of the abdomen, which demanded a study of anatomical relations which had never been taught in the schools."
Dr. Theodore McGraw was focused on both teaching and learning, and that desire is summed up in this quote "We entered into the matter with unbounded enthusiasm – enthusiasm for teaching and developing ourselves."
To this end, the charter of the Detroit Medical College elucidated how this would be achieved. In the charter (pictured below), it is written that "Pains will be taken to instruct each Student in PRACTICAL DIAGNOSIS. For this purpose the advanced Students will be called upon in turn to examine patients. After pronouncing a Diagnosis, questions will be asked in relation to differential symptoms... ...Little benefit can result to the Student from seeing cases diagnosticated and treated by the Professor of Practical Surgery and Medicine, unless he is first allowed to exert his own powers, and test his own knowledge, by personal examination of the patients."
The Detroit College of Medicine charter from 1868, signed by founding physician Thodore A. McGraw, MD. The charter puts forth the founding principles of the institution.
This ethos of having students practice medicine, to serve the community, and to learn by doing, echoes throughout the history of the School of Medicine. This is the very foundation of the University and the key to its enduring greatness. It is also the reason that I chose to attend WSU SOM - I wanted to immerse myself in the diversity of the city and the breadth of clinical opportunities available in Detroit, from serving homeless and uninsured patients in community clinics to learning from some of the leading minds and researchers in the country at the University clinics.
At its inception, the Detroit Medical College set up a relationship with Harper Hospital and St. Mary's Hospital, which allowed students to learn from and serve the people of Detroit. The focus is, and has always been, learning by doing. The early photos below illustrate these tenets.

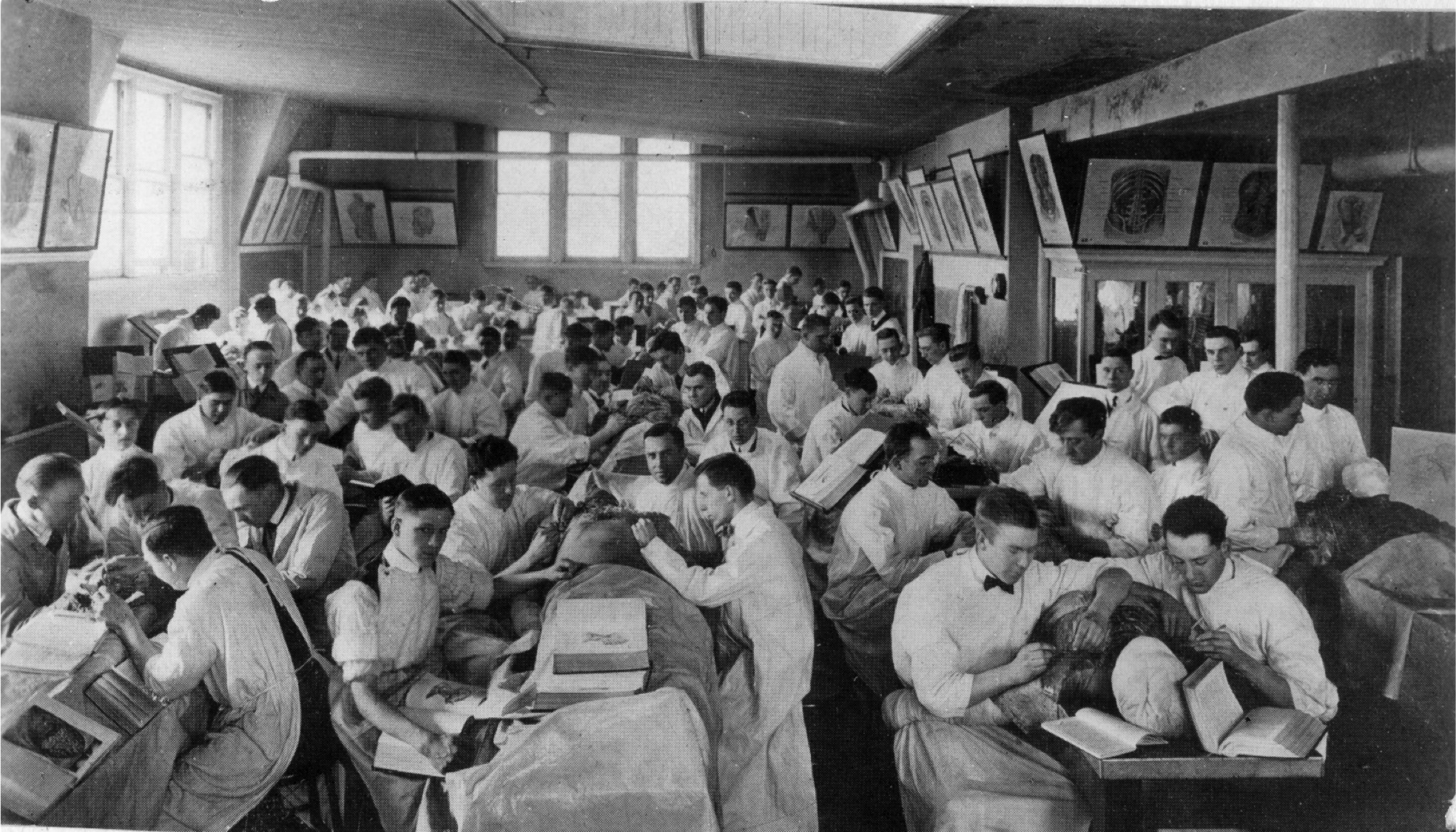
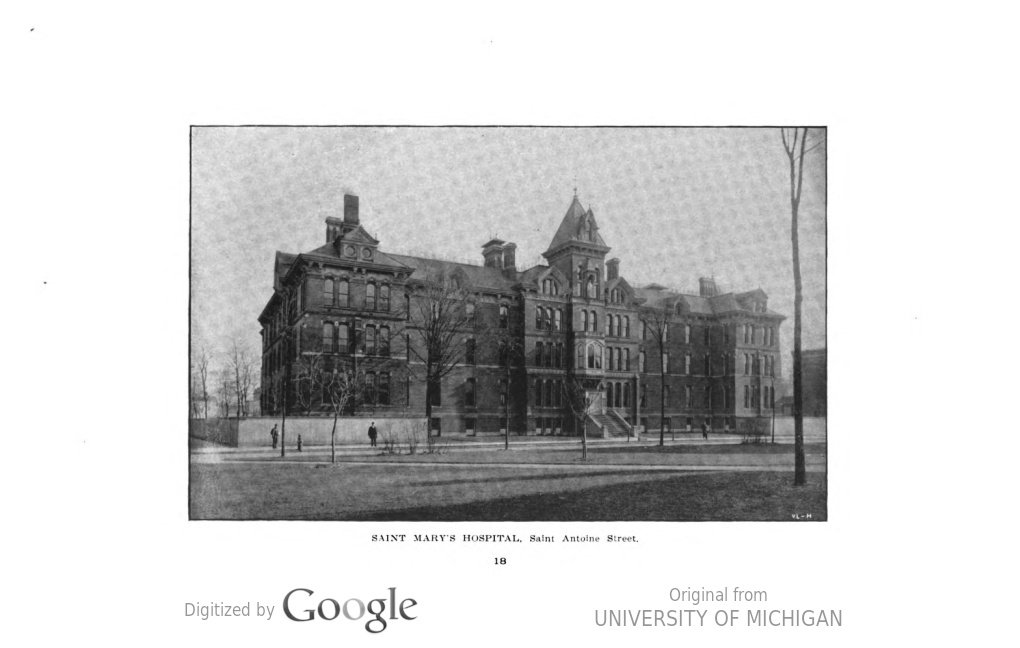
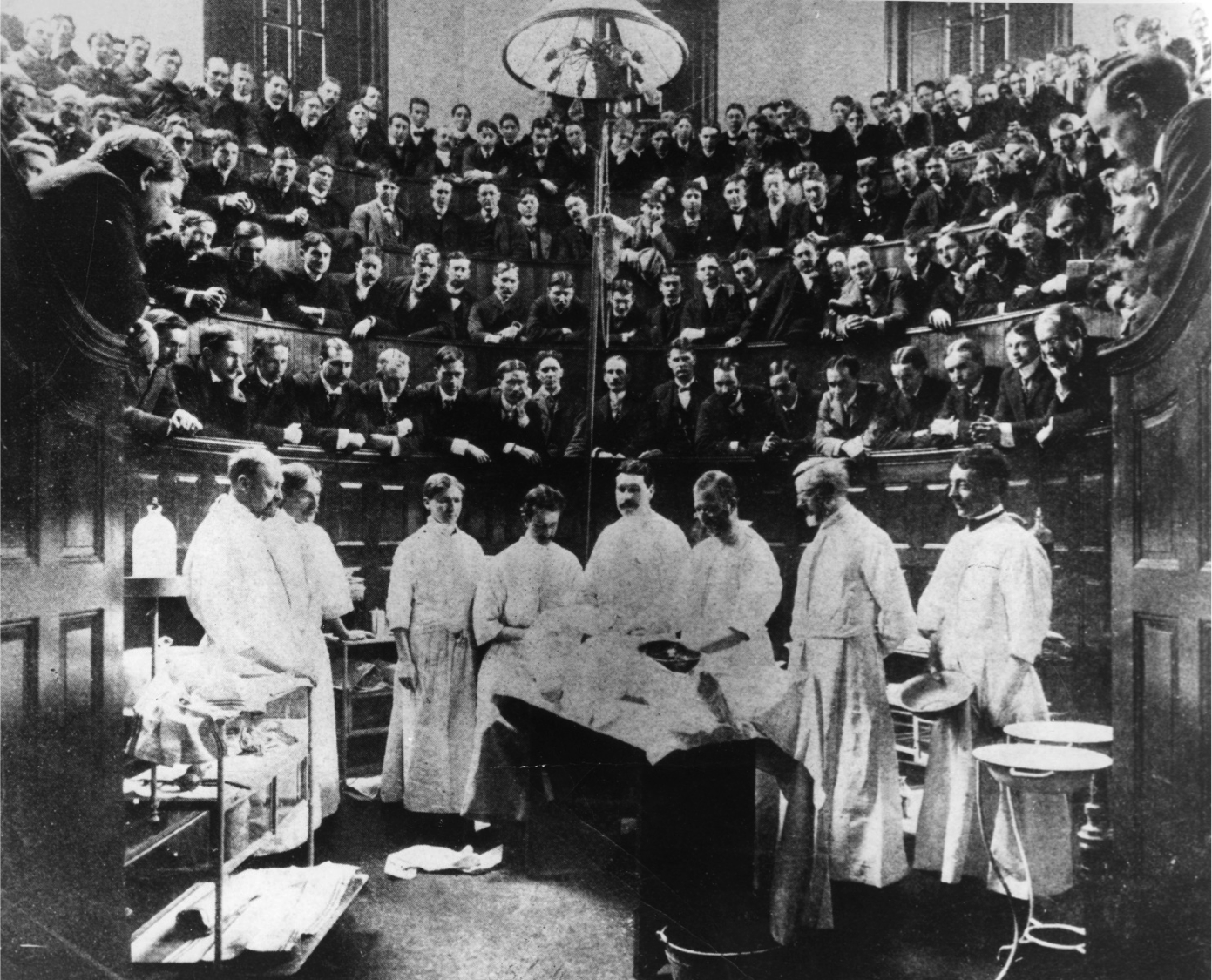
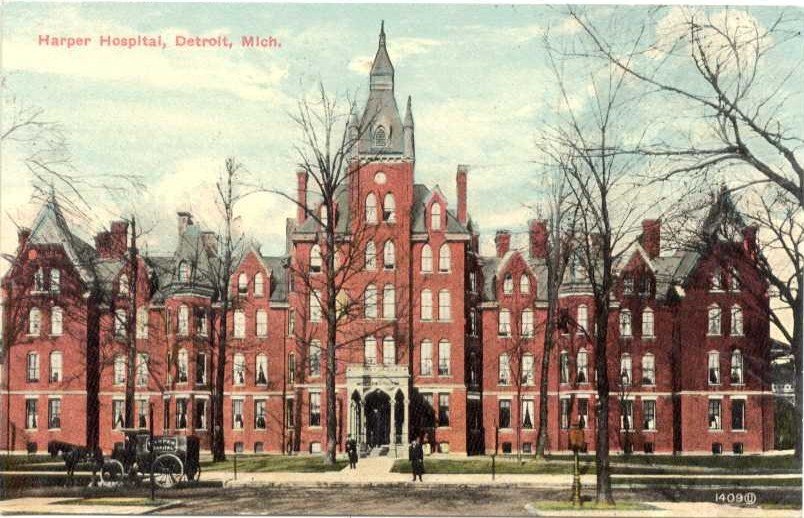
The above photo series include the following images: first is the Detroit Medical College, which housed the medical school after 1868, the second image shows students during anatomy lab sometime around 1900, which is not very different than anatomy lab at the School of Medicine today. The third image is St. Mary's Hospital, one of the two clinical training sites after 1868. The fourth image is the operating theater at St. Mary's Hospital in 1898. The Operator is Dr. Henry O. Walker. At his left, hands behind his back, is Dr. Theodore McGraw, the founder of the Detroit Medical College who emphasized teaching by doing. The final image is Harper Hospital, the primary clinical training site for students at the Detroit Medical College.
It was an honor to be able to relay the history of Wayne State University School of Medicine to my physician colleagues this weekend, and it is a great reminder of what makes doctors from Wayne State unique and so skilled - the focus on hands-on clinical training and the diversity of the people we have the privilege of serving.

Thanks for reading,
- Dr. Paul Thomas, Physician with Plum Health DPC
Plum Health on Bonfires of Social Enterprise
Last month, I had the pleasure of being interviewed by Romy Kochan on her podcast, Bonfires of Social Enterprise. Bonfires of Social Enterprise is focused on highlighting social entrepreneurs and we were happy to be featured on this podcast!
I believe that Plum Health DPC is a social enterprise because we not only focus on growing the business in a traditional sense (revenue, profit & loss, etc...), but we also focus on making a positive impact in the community by providing a medical service that is much needed the SW Detroit community.
Romy was a great interviewer and made me think differently about my own practice, prompting me to say something I've never said before. She asked if I could dream big, and envision a future for what I'm doing, what could this look like?
I responded by saying, "I think this could look like a nation where we get rid of these old notions of what 'good health care' looks like, and starting to realize that it doesn't look like a piece of plastic in our wallet. It looks like a relationship with someone in our community that is a healer, that can listen, and has time to address your concerns".
The conversation had a broad scope from how we got started, to the impact we're having, to the reaction to our service from the community. Here's how Romy describes it:
We’re back with another episode here on social enterprise. We have a doctor on this show who has been making a big impact in Detroit. It is Dr. Paul Thomas of Plum Health Care DPC. He has a dream of changing the notion of health care from a plastic card in your wallet to true healing from a healing doctor! What a concept!
This was a wonderful interview and I am so grateful to Romy Kochan for having me on her podcast. Check out the full episode here, and have a healthy week!
- Dr. Paul with Plum Health DPC
PS: you can find this episode on the podcasting platform of your choice:
PRX.org (Public Radio Exchange)
PPS: Follow us on Instagram!
Plum Health with the Black Health Academy
Last month, we had a great visit from and interview with Lisa A. Smith with the Black Health Academy. We first met during a small business course with the Build Institute in Detroit, and it was great getting back together for this interview! She has a passion for health and wellness and helping people reach their full potential. Here's how she tells her story on her webpage:
Lisa A. Smith, MBA, is the founder of Professionally Fit INC and The Black Health Academy. She began her own weight loss journey in 2012 at 190 lbs. She fell in love with fitness, nutrition and self-development, lost over 60 lbs and gained a bottomless amount of confidence. It wasn't until she gained confidence in her physical health that she was able to gain confidence in her career. With her new found confidence she launched Professionally Fit in July of 2015. Professionally Fit is an executive coaching platform which provides both the customization and accountability necessary for high performing entrepreneurs and executives to achieve their health and wellness goals from anywhere in the world.
Health disparities in detroit
Our conversation focused on health and wellness in the black community. There are almost unbelievable health disparities between white Americans and black Americans, and we discuss some of these differences during our interview. Lisa also highlights these disparities on her website:
Here are the facts:
- 47.8% of African Americans are considered overweight or obese
- African Americans are 20% less likely to be treated for depression
- 13.6% of African Americans have fair to poor health
- 40.9% of black men over the age of 20 have high blood pressure
- Heart disease, cancer and stroke are the leading causes of death in the black community
Topics covered during our masterclass
During our Masterclass, we discuss these health disparities, what inspired me to become a physician, the community-focused efforts at Wayne State University School of Medicine, why other physicians might not practice in a more community service-oriented way, what Plum Health is, how we manage the volume of patients in our practice, our range of services or scope of practice, the type of feedback that we've been getting from our members, trends in African American health, on not making assumptions about people's health and meeting people where they're at, and on making lifestyle recommendations versus taking medications.
I really loved this interview with Lisa A Smith - it was like siting down with an old friend. If you want to learn more about her and what she does, please visit the Black Health Academy or follow her on Facebook.
Thanks for reading and watching, and have a wonderful day!
- Dr. Paul Thomas with Plum Health DPC
PS Follow us on Instagram!
Plum Health on Daily Detroit
This week, we were featured on the Daily Detroit Podcast. It was great meeting up with Sven Gustafson and Jeremiah Staes, the journalists behind the publication, and hosting them in our office in Southwest Detroit.
You can listen to the full episode here:
Here's what Sven Gustafson wrote about our practice, in the context of the interview:
Dealing with health insurance is few people’s idea of a good time — if you can afford it at all, that is.
Now, a doctor operating out of an office in a former Detroit Police Department precinct headquarters? That’s flipping the script on the traditional model of health care.
On this episode of the Daily Detroit Happy Hour podcast, we schedule an appointment with Dr. Paul Thomas of Plum Health in Southwest Detroit. He’s practicing a model known as direct primary care in which patients pay a membership rate, starting at $10 a month for children and climbing to $89 a month for seniors, directly to the doctor. In exchange, patients get more personalized care, better access and lower-cost medications, imaging and laboratory services.
Dr. Thomas, who graduated from the Wayne State University School of Medicine, estimates he can cover 80 to 90 percent of most people’s health care needs. So he acknowledges it’s not a complete solution to our country’s problem-plagued health care system.
We talk to Dr. Thomas about how direct primary care works, how it differs from traditional insurance-directed health care and how it affects both patients and his life as a working physician. He also tells us about the various ways he’s using digital technology to facilitate his job and market his business.
Find us and subscribe on Apple Podcasts or wherever fine podcasts are downloaded. Previous episodes are here.
Daily Detroit's tagline is "what to know and where to go in Detroit" - it's worth knowing more about Detroit, if you're a resident, a Metro Detroiter, or from another part of the world. Sven and Jeremiah cover interesting stories and give great insights, so their podcast is worth a listen/subscription.
Thanks for reading and listening, and have a wonderful day,
- Dr. Paul Thomas with Plum Health DPC